Peter Hotez on Patent-Free Vaccines—and Texas, Tito’s, and Twitter
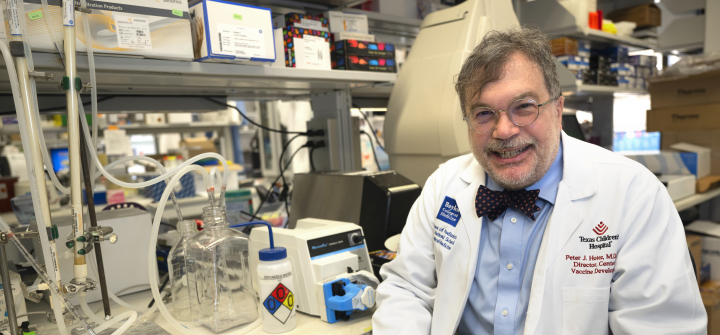
Peter Hotez—with his signature uniform of lab-coat-and-bow-tie—has been a prominent voice on vaccine equity and misinformation throughout the COVID-19 pandemic.
Amid a global vaccine race that led to colossal windfalls for Big Pharma and left poor nations behind, Hotez’s team created a patent-free COVID vaccine that has already begun filling vaccine gaps around the world. And a new bivalent booster is in the works.
Hotez, co-director of the Center for Vaccine Development at Texas Children’s Hospital and dean of the National School of Tropical Medicine at Baylor College of Medicine, spoke to GHN about patent-free vaccines, as well as Twitter, Texas, and Tito’s vodka.
His latest book, The Deadly Rise of Anti-Science: How Health Freedom Propaganda Endangers the World, comes out soon.
What’s the latest on your patent-free COVID vaccine? How many people has it reached?
Our recombinant protein COVID vaccine technology has been licensed to 4 major entities, and 2 that have scaled it up into vaccine production: Biological E in India and Biofarma in Indonesia. Between them, we’re hitting the 100 million dose mark. The technology has also been transferred to Botswana and Bangladesh.
It’s a validation that you don’t have to be a Big Pharma company to do big things.
That’s very important because we need to pay greater attention to our low- and middle- income country vaccine producers if we’re ever going to hope to decolonize the vaccine ecosystem.
The FDA has announced a potential long-term strategy involving annual COVID boosters. This is going to be the next phase of vaccine inequality—boosters that will be made available for North America and Europe, and not necessarily the rest of the world.
So my team is working on bivalent version of our COVID vaccine as well.
How can more countries to take advantage of patent-free vaccines?
India and Indonesia had existing infrastructure that we built on. Other countries do, too.
Maybe a dozen LMICs make their own recombinant protein hepatitis B vaccines using microbial fermentation and yeast. It’s an old-school technology.
Our strategy is to develop our vaccine technologies that allow us to plug-and-play into their system.
If and when companies in India and Indonesia receive WHO prequalification for the vaccines being produced there using our technology, those vaccines could be sent anywhere in the world—but WHO has been sitting on prequalification for months and months.
That’s an indication that we’ve got to come up with alternative regulatory systems—not have everything go through the WHO pipeline. They don’t have the bandwidth to process all of the applications in a timely way.
What other barriers are you running into?
Part of the problem is everyone is so focused on speed and innovation. Those are important, but they put a velvet rope around the Pharma companies.
When it came to COVID vaccines, no one had that situational awareness—apart from organizations like ours—to say “Wait a minute, if your vaccine technology isn’t compatible with the LMIC vaccine producers, it’s going to leave a lot of people living in poverty on the outside looking in.” That’s exactly what started to happen during the COVID pandemic.
I don’t think we should demonize Big Pharma either. They do a lot of good, providing vaccines for the Gavi vaccine alliance to globalize vaccines and immunization. But we saw what happened. In 2020 and 2021, my team received frantic phone calls from science and health ministers in LMICs when they realized the mRNA vaccines weren’t coming anytime soon.
We’ve become over-reliant on the multinationals at the expense of the LMIC vaccine producer. Our approach helps balance out the ecosystem by having alternative pathways.
Could this approach usher in a different model for vaccine development overall?
Absolutely, and particularly for the vaccines that pharma companies would have no interest in making. We’re also involved in making vaccines for parasitic diseases that are of local or regional importance but not global importance.
Pharma companies are never going to make vaccines for hookworm or Chagas disease. We’re making those vaccines. Hopefully we can provide a model for a whole pipeline of vaccines for global health.
You recently tweeted that your work relies on philanthropy. Is that how it should be?
Globally, we really haven’t made a serious effort to try to fix vaccine inequality. We need greater direct support from the G20 countries. In this emergency, we were cut out of Operation Warp Speed because we’re not a Pharma company.
But local philanthropy in Texas really came to our rescue—organizations like the Kleberg Foundation, and even Tito’s vodka, were instrumental.
We didn’t raise the billions that Moderna and Pfizer got through taxpayer money and advance purchasing—but it goes to show you could do a lot with millions.
It’s one of the reasons we came to Texas, which people often don’t realize has a very strong scientific environment and is a very philanthropic state. If we hadn’t come to Texas. I don’t know that we could have done this patent-free vaccine—because of the resources here.
You’ve been open about harassment and threats you’ve received, including recent images depicting a swastika made up of syringes that was sent to your home. What role does anti- vaccine disinformation play in these incidents?
Standing up to that kind of aggression, it’s as important as making vaccines. Anti-vaccine activism is one of the biggest barriers to vaccines reaching US populations.
US-style anti-vaccine aggression is now reaching Canada, Western Europe, and LMICs on the African continent and in South Asia.
This is a major problem for all vaccines, including childhood immunizations.
Do you think this behavior will recede as the pandemic does?
It’s not getting better. It’s about to get worse. The House oversight and the House judiciary committees have announced investigative hearings around COVID origins and vaccines. It’s going to be a war against biomedical scientists. We’ve got to get ready and try to educate our scientific societies and our national academies around this.
I understand that whenever possible, we need to be politically neutral, but to paraphrase Desmond Tutu or Eli Weisel, sometimes neutrality favors the aggressor, and that’s what’s happening here.
You’re very active on Twitter, responding to and debunking misinformation. How do you choose what to respond to, and what to ignore?
It’s become a minefield. That’s not been fun.
Mostly I mostly engage with elected leaders who are openly and brazenly espousing anti-vaccine rhetoric—like Rep. Marjorie Taylor Green from Georgia. She has a lot of power and influence. People identify with it and are not getting vaccinated because of their political leanings.
I try to use Twitter is an educational tool because too often people think of this anti-science aggression as random misinformation, or disinformation, or [an] infodemic. These are really euphemisms. It’s not random. It’s organized, and it’s politically motivated.
Anyone’s entitled to their views—even extreme conservative views—but we have to uncouple the anti-vaccine activism from that because it’s just killing too many people.
This interview has been edited for length and clarity.
Join the 50,000+ subscribers in over 170 countries who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues.
Peter Jay Hotez, M.D., Ph.D.