‘Gardeningʼ in the Gut: Tackling Antibiotic Resistant Bacteria With Vaccines and Friendly Bacteria
The pipeline for new drugs to fight antibiotic resistant infections is rife with challenges, but there’s a promising solution on the horizon—and it doesnʼt involve antibiotics.
A Science study published in April demonstrated in mice how highly effective oral vaccinations can be combined with harmless bacteria that outcompete the bacteria for food and “starve them out.” The research focused on Escherichia coli and Salmonella, two common infections that have seen a rise in drug-resistant infections.
The method is a lot like weeding a garden, explains Emma Slack, PhD, a professor at ETH Zurich and the University of Oxford’s Sir William Dunn School of Pathology.
“If you pull out all the weeds, you go back three days later and all the weeds are there again. If you don’t want that to happen, you’ve got to put something in the place where the weeds would grow,” Slack told GHN.
The novel intervention tackles pathogenic microbes in the gut without the need for antibiotics, and homes in on reservoirs where drug-resistant bacteria can linger before they cause symptoms.
GHN spoke with Slack about how the method works, its potential to help tackle the global crisis in antimicrobial resistance, and its wide-ranging possible clinical applications.
Where did the idea for this research come from?
My postdoctoral work focused on how the immune system in the intestine works. We found that when we made vaccines that induced a strong response in the intestine, we were getting good protection from bacterial infections for around 24 hours and then the bacteria would evolve to escape.

Thesis-cover: Electronic art depicting flagellated bacteria swimming between different types of antibodies. Courtesy of Emma Slack
Because bacteria in the gut are very numerous and they grow very fast, they can evolve very quickly. And we were getting very, very rapid, immune escape from these vaccines.
We realized that the vaccines weren’t so much just protecting, they were influencing the outcome of competition between genetic variants of bacteria that were arising in the intestine.
So the idea was—instead of waiting for genetic variants to naturally appear—to put something into the gut that can take that role [of the genetic variants] from the beginning. Then you can use antibodies that you induce with the vaccine to manipulate the competition between a pathogen and this other friendly bacteria species that you’re adding, such that the friendly bug always wins that competition.
Why combine a vaccine with harmless bacteria?
The gut is not a naturally sterile environment. It’s an open system that’s very heavily colonized all the time.
Currently, most bacterial vaccine approaches are focused on preventing disease, which is great. But they often don’t act at the level of colonization in the gut.
If you kill bacteria in the bloodstream, for example, they’re gone. Whereas in your intestine, if you if you kill bacteria, you generate a friendly environment that more bacteria can grow in.
In the gut, antibodies don’t really kill bacteria. All they do is stick them together into these big aggregates that get moved out of the gut much more quickly.
But the problem is still that because it’s an open system. If you clear something out more quickly, potentially, it can just grow more quickly to fill up the space that is being vacated.
How significant was that difference between using the harmless bacteria and the vaccine by themselves, and using them together.
It’s huge, actually. With a vaccine alone or the harmless bacteria alone, research has shown that you can drop pathogen loads by maybe 100,000-fold. If we put them together we can get them down to more than a 1 billion—so 10,000 times more potent than the individual components alone.
What are the most exciting possible outcomes of this method?
Weʼre probably five to 10 years to get the first clinical uses, but I think the most exciting thing is this potential to reverse the antimicrobial resistance crisis for gut colonizing, opportunistic pathogens.
How could this approach reduce the use of antibiotics or prevent antibiotic resistance?
If you survey a standard population of healthy humans, you find quite a lot of uropathogenic E. Coli—E.Coli that causes urinary tract infections–in the gut.
These strains are far more numerous in the guts of humans than they are in the urinary tract. A decent fraction of those will be also antibiotic-resistant, and they can cause bloodstream infections. If we could vaccinate against them at the population level, it would enormously reduce the incidence of E.Coli-driven urinary tract infections.
That would involve quite a lot more work, because thereʼs a big diversity of strains and weʼd need to understand the metabolism of those strains, how to design competitor bacteria, and how to make the vaccines. But long term that that would be really exciting. One day, people may be able to swallow a capsule that contains the vaccine and the competitor bacteria.
What are other possible clinical applications?
Anything where immunosuppression is one of the side effects, which gives people this high risk of getting bloodstream infections and can ultimately lead to deadly antibiotic resistant bugs. Any sort of transplantation is relevant.
For example, using this method we could try to come up with a two-to-three-week treatment before a transplant procedure that clears the antibiotic-resistant E.Coli, and ideally also Klebsiellas, from the gut. [This] would result in a much lower risk of developing an antibiotic-resistant infection.
We’ve also been looking at high-risk pregnancies, because babies born prematurely are at very, very high risk from E. Coli-driven sepsis and meningitis. And if we can treat mothers with very safe oral vaccine treatments that could be an easy, very useful application with a real impact.
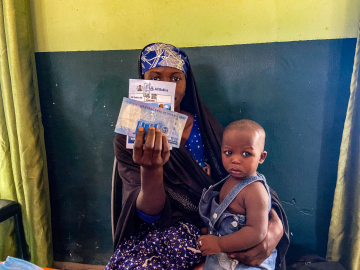
How accessible would this method be in low- and middle-income countries, and what are the challenges there?
The vaccines we’re using are similar to the oral cholera vaccine. They’re very stable and storable at room temperature. You don’t need a doctor to administer them, and they’re easier to transport. So they have all sorts of benefits for global application compared to a live, injected vaccine which requires cold storage.
One challenge is that these applications are going to be bacterial strain dependent. Often our knowledge on the types of circulating strains and the diseasecausing circulating strains in low- and middle-income countries is far less compared to just our understand of what strains are circulating in the U.S. or Europe.
So, there is a need not only for product development, but for epidemiological studies in those regions to know exactly what we’re targeting.
Join the 50,000+ subscribers in 170+ countries who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues: https://www.globalhealthnow.org/subscribe.
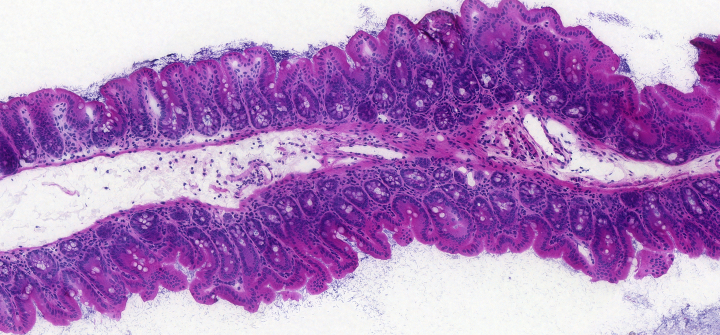
622A_cecum: Section through a healthy mouse cecum stained with Haematoxylin-eosin. Courtesy of Emma Slack