How COVID-19 Set Back India’s Battle with Leprosy
MADURAI, India—He found Karupayee hunched listlessly on the floor in a corner of her room. Outside, it was a bright, windless morning in this Southern Indian city. Her home, a 6x8-foot shed with a slanting, corrugated iron roof, was found at the end of a winding mud path. The door and windows were shut. It was pitch dark inside.
It was around 11 a.m. on August 23, 2021. After months of COVID-19 lockdowns, M. Raja and his team from the Madurai Health and Leprosy Relief Centre (Mahelerecen) could finally pay a visit to Karupayee, who goes by only one name.
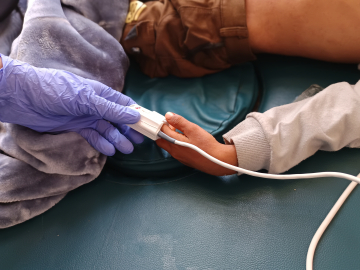
Raja, a coordinator for the nonprofit that rehabilitates leprosy patients, had known Karupayee for years, ever since she had been diagnosed with grade 2 leprosy that had caused severe deformities in her fingers and toes.
A chronic, infectious disease when left untreated, leprosy is caused by the bacteria Mycobacterium leprae, which is likely transmitted via droplets through prolonged, close contact with infected, untreated patients. The slow-moving disease may take years for infected people to experience symptoms. Eventually, numb, discolored patches spread over the skin. Tiny nodules and lesions develop over the feet, body, and arms. Muscle weakness and paralysis, eye problems, as well as the shortening of toes and fingers, often follow.
Karupayee had been cured in 2007 after a 2-year course of multidrug therapy. (The treatment has been provided by the pharmaceutical giant Novartis since 2000 through the WHO.) The multidrug therapy has been a game-changer, curing thousands of patients of the disease—though many of them still must deal with severe disabilities. Peripheral nerve damage had caused a loss of sensation in Karupayee’s fingers and toes, which led to shrinking of these digits—a common outcome in leprosy patients that gives the hands a claw-like appearance.
In the years after Karupayee, 67, was treated and her leprosy was cured, Raja helped her find work, arranged for food at nearby shelters, and ensured that she took her medicine. After she could no longer work as a cleaning lady, she collected odds and ends to recycle as a rag picker.
Then the pandemic hit. Lockdowns were instituted. And, for the first time in 15 years, Raja had lost touch with the people he served.
India’s 2 deadly waves of COVID-19 are estimated to have killed 4 million people by June 2021, but intermittent lockdowns took a separate toll on Indians with leprosy. Detection, treatment, and rehabilitative services were severely disrupted.
One indication of COVID-19’s impact on leprosy screening in India is the sharp reduction in the number of new leprosy cases detected. In 2019-2020 during the year before the pandemic, 114,451 new cases were recorded, according to the government’s official count. But in 2020-2021, only 65,147 new cases were detected, according to WHO.
At the Leprosy Mission Hospital in Dayapuram, Manamadurai, for example, daily patient screenings fell from 150 to 10 during the first wave’s March 2020 lockdown, says Jaquline Jose, a dermatologist and medical superintendent.
Screening is critical because it can lead to early treatment that prevents disability, and it also reduces community spread. But detecting leprosy in lower-income communities is especially challenging because many daily wage earners “don’t have the privilege to stop a day’s work to investigate a lesion or a white patch,” Jose says. “So, these early symptoms are often ignored until the disease is advanced.” The lockdowns made screening in lower-income communities even more difficult.
Another pandemic impact: footwear. For a leprosy patient who is cured, finding a job with a stable income is often a major challenge, and a surprising essential for many is custom-made sandals.
Since leprosy affects the nerves, patients often develop painless ulcers, lesions, and sores on the feet that cause damage to tissues and bones. This can affect their ability to walk. To deal with these problems, many rely on specialized footwear. The entire sandal is made from microcellular rubber and is springy and soft, with custom-made insoles that can ease pressure on foot ulcers by redistributing body weight, says physiotherapist Preethi Suresh. At Dayapuram, the footwear is provided free to every leprosy patient. Before the pandemic, Dayapuram’s cobbler, M. Pandi, produced up to 1,000 pairs per month. Then COVID-19 disruptions ground his production to a halt. He is just now getting closer to his pre-COVID production capacity.
The lockdowns also meant that follow-up care for patients and survivors suffered. For Raja and his team, the lockdowns made it impossible to continue regular appointments with people like Karupayee. When he was finally able to see her last August, he knew instantly that something was wrong.
“Who are you?” she asked, while staring blankly right past him. Cataracts in both her eyes had dimmed her vision, but without support, she had no options for eye care as her world became darker. Neighbors looked in on her during the lockdowns and provided her with some meals, but she was essentially starving.
One of the pandemic’s worst impacts on people with leprosy might be the sheer isolation. A nephew’s weekly visits to Karupayee, apparently dropped off during the lockdowns. Her health (and especially her vision) deteriorated when she had little contact with others. Raja found it difficult to get a relative’s consent for Karupayee’s cataracts surgery at a tertiary care hospital, even though it would be done for free. After numerous attempts, her nephew finally gave his consent on the morning of the surgery.
Now, Karupayee doesn’t stay locked up at home anymore. Though she still needs one more cataract surgery in the other eye, her vision has significantly improved.
“It’s been a long struggle, but the world is a brighter place for me now,” she says.
Read part two of this series here.
Kamala Thiagarajan is a freelance journalist based in Madurai, Southern India.
Ed. Note: This article is part of Global Health NOW’s Local Reporting Initiative, made possible through the generous support of loyal GHN readers.
Join the 50,000+ subscribers in over 170 countries who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues.
Karupayee with M. Raja (middle) and A. Vincent of the Mahelerecen Leprosy center in Madurai, India. March 3, 2022. Kamala Thiagarajan