Neglected Tropical Diseases: A Lesson in Elimination?
It’s the global health world’s ultimate goal: disease elimination.
After the eradication of smallpox in 1979, the global health community set its sights on several other deadly diseases, including polio, TB, and malaria. Comprehensively beating diseases like these is a complex, time-consuming undertaking—Sustainable Development Goal 3 targets 2030 for ending the AIDS, malaria and TB epidemics.
But for a group of neglected diseases, elimination is within reach—thanks in large part to better diagnostics—an “unsung hero” of global health.
On January 30, 2012, donor agencies, pharmaceutical companies, research institutions, NGOs, governments, and other global health stakeholders signed the London Declaration on Neglected Tropical Diseases, endorsing the WHO “NTD Roadmap” (Accelerating Work to Overcome the Global Impact of Neglected Tropical Diseases) and committing to control, eliminate or eradicate 10 diseases by 2020.
As a group, NTDs affect more than 1 billion people—and cost economies billions of dollars—annually. These diseases were historically overlooked, largely because they thrive in conditions of poverty. While the ambitious 2020 targets may not all be reached, the London Declaration gave critical momentum to the fight—spurring increases in funding, advocacy and expertise. 8 years on, the first World NTD Day, January 30, 2020, provides a much-needed boost for NTD control and elimination.
Have these efforts helped? Back in 1995, a WHO Expert Committee estimated that 300,000 new infections of human African trypanosomiasis (HAT; commonly known as sleeping sickness) occurred annually in Africa—with fewer than 10% of all cases diagnosed and treated. The WHO NTD Roadmap targeted global elimination of sleeping sickness as a public health problem by 2020; by 2018 the number of cases reached a historic low (<1000). Today, several countries including Uganda and Ivory Coast are close to getting their HAT elimination status validated.
Lessons from the NTD community’s approach—including the critical role of diagnostics—could accelerate progress against other diseases, such as TB and malaria. Diagnostics are imperative for disease surveillance, with large-scale screening initiatives needed to track down the last cases, as a crucial complement to treatment strategies, and to block transmission.
For sleeping sickness, the development and deployment of rapid, point-of-care tests that can track down infections in remote, hard-to-reach areas proved a game-changer—increasing the chances of early diagnosis, facilitating treatment, and stopping transmission.
The ease-of-use of these tests has made it possible to ensure testing access for entire at-risk populations. Combined with the availability of improved treatments (like the recently approved fexinidazole, an oral medicine) they are transforming sleeping sickness—a once-dreaded disease that only specialized health facilities could handle—into an illness manageable in the decentralized, primary care settings where most patients initially seek care.
Other efforts to decentralize diagnostics show promising impact, too—including rapid diagnostic tests for malaria and HIV self-testing. Higher-sensitivity urine antigen detection tests are now emerging for the rapid detection of TB among people living with HIV.
In 2018, WHO acknowledged the critical importance of diagnostics in achieving universal health coverage, releasing the first-ever Essential Diagnostics List and an updated edition in 2019—sending strong signals that diagnostics are as important as essential medicines. The upcoming Lancet Commission on Diagnostics will hopefully advance the agenda.
The right diagnostics implemented efficiently within health systems so that they are available where patients seek care is a familiar refrain—but one that cannot be repeated enough.
On this first World NTD Day, we congratulate the NTD community on its impressive achievements and champion the efforts needed as the last mile comes into view. We encourage the global health community to learn from these experiences and acknowledge the importance of investing in diagnostics so that we can hit the SDG targets and consign more deadly diseases to the history books.
Catharina Boehme, MD, is CEO of the Foundation for Innovative New Diagnostics (FIND).
Joseph Ndung’u, BVM, PhD, CorrFRSE, is Head of Neglected Tropical Diseases at FIND, Chair of FIND Kenya, and Chancellor of Jomo Kenyatta University of Agriculture and Technology (JKUAT).
Madhukar Pai, MD, PhD, is a Canada research chair in Epidemiology and Global Health at McGill University in Montreal, director of McGill Global Health Programs and director of the McGill International TB Centre.
Join the tens of thousands of subscribers who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday enewsletter, and please share the link with friends and colleagues: https://www.globalhealthnow.org/subscribe
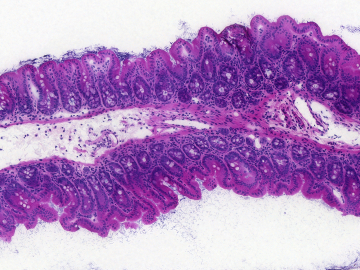
Active screening for sleeping sickness in Democratic Republic of the Congo. Photo credit: FIND/Ndung’u 2018