A Roadmap for Ending the Moral Catastrophe of TB
The good news is that tuberculosis deaths are declining steadily. The bad news is that we are wildly off track to meet the bold targets set for controlling the world’s #1 lethal infectious disease.
The Sustainable Development Goals call for a 90% reduction in TB deaths by 2030.
And the WHO’s End TB strategy calls for a 90% reduction in TB incidence by 2035. Yet at current rates of decline, a 90% reduction in TB incidence probably will not be achieved in in India until 2124 or in Uganda until 2134, for example.
Such slow progress inevitably means an enormous burden of suffering and mortality. Yet TB is preventable, treatable and curable—making the avoidable burden of TB a moral catastrophe.
Fortunately, there is a growing momentum to address the lack of progress.
In September 2018, all 193 UN member states adopted a political declaration on TB committing them “to accelerate national and collective actions, investments and innovations in fighting the preventable disease.” Translating that declaration into concrete action requires a roadmap for how high-burden countries and their donor partners should prioritize investments toward ending the epidemic. The Lancet Commission on Tuberculosis Report, published this week by an international group of 76 authors, including ourselves, provides that roadmap.
The report, Building a Tuberculosis-Free World, highlights the critical importance of scaling up proven TB control strategies, such as TB preventive therapy, drug susceptibility testing (so that patients receive the right treatment), and second-line drugs to treat drug-resistant TB. Improving the quality of TB care is also essential. The commission found that in India alone addressing poor quality care, especially in the private sector, will save more than 8 million lives over the next 25 years. Failing to implement these proven strategies in high-burden countries has huge economic consequences: In India alone, failure to achieve the SDG targets costs the economy $32 billion every year.
The report highlights that increased investment in TB control is likely to bring large economic returns. For example, the commission estimates that the benefit-to-cost ratio for TB interventions is 7:1. Greater domestic resource mobilization, especially in middle-income countries, will be key. Countries such as Bangladesh, China, Indonesia, and Zambia could increase their annual TB expenditures more than 5-fold over the next 5 years through increased revenue generation and allocation of greater budgetary resources to health.
To accelerate progress, we also need new TB control technologies. While the Stop TB Partnership estimates that it will take an annual investment of $2 billion to develop critically needed products, we are only spending around $700 million per year. Closing the funding gap for TB product innovation will require all countries, especially high- and middle-income countries, as well as the private sector, to increase their investments.
Finally, the report underscores the importance of accountability to ending the epidemic. Establishing greater accountability at all levels, from heads of state to the local TB clinic, is necessary to ensure that promises are kept and targets reached. To this end, the commission plans to launch a “TB Observatory” to track progress toward global targets. Meeting annually over the next 5 years, the Observatory will evaluate country progress towards global targets and ensure that the report’s recommendations lead to urgent policy changes, helping high-burden countries develop strategies to address their TB epidemics and also to secure universal health coverage.
Many countries, including China, Cameroon and Ethiopia, have achieved substantial declines in TB mortality over a 20-year period. Other countries could achieve similar results. With bold leadership, shared responsibility, and smart investments based on sound science, we can end TB within a generation.
Michael Reid is an assistant professor of Medicine in the School of Medicine at the University of California, San Francisco and also works at the UCSF Institute for Global Health Diplomacy and Delivery. Twitter: @MikeReidMD
Gavin Yamey is a professor of Global Health and Public Policy at Duke University, where he directs the Center for Policy Impact in Global Health at the Duke Global Health Institute. Twitter: @gyamey
Join the tens of thousands of subscribers who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday enewsletter, and please share the link with friends and colleagues: http://www.globalhealthnow.org/subscribe.html
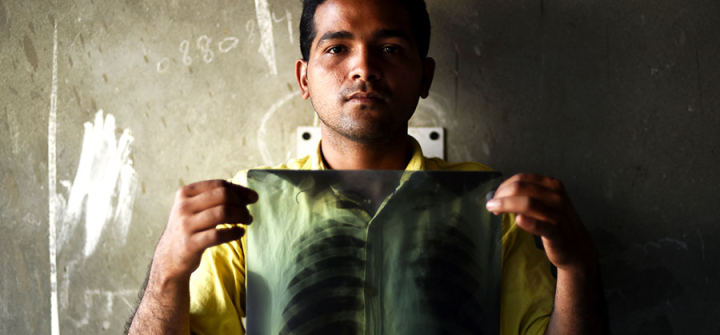
Indian TB patient Sonu Verma, 25, poses with his chest x-ray in Sonipat, March 3, 2016. Image: Money Sharma/AFP/Getty