A Promising Fight Against a Silent Killer
LODWAR, Kenya—In the sweltering children’s ward at Lodwar County Referral Hospital (LCRH), the air hangs heavy as frail children lie on narrow beds, some asleep, others restless. Their tiny bodies are locked in battle with kala-azar, also known as visceral leishmaniasis.
On their weak wrists, thin plastic cannulas are taped in place, a constant reminder of the daily injections they must endure to survive the parasitic disease.
Caregivers—both mothers and fathers—at the hospital in Turkana County are both weary and resolute. Many have left their other children at home with relatives or older siblings while they stay in the hospital with their ailing children.
To escape the ward’s oppressive heat, caregivers retreat outdoors. Some cradle their children in their arms, while others look out over the vast landscape, their thoughts heavy with the fear of losing their child to kala-azar.
“Three children died here recently,” says caregiver Pamela Ekutan, her voice heavy with grief. “It’s frightening, but we hope our children will get better.”
Amid the fatigue and worry among caregivers at the LCRH, an unspoken solidarity, a quiet strength binds them together. For those whose children are nearing the end of their lengthy treatment for the disease, hope begins to bloom, faint but steady. For others, the road ahead stretches long and uncertain.
Ekutan, a mother of four, is among those waiting anxiously. Her 5-year-old son Lomoe has been hospitalized for two weeks, undergoing treatment for kala-azar. The doctor has told her that Lomoe’s immunity must stabilize before he can receive a blood transfusion.
“It started like malaria—fever, fatigue, low appetite,” Ekutan says. “I took him to the dispensaries, but the symptoms persisted. That’s when I brought him here and found out it’s kala-azar.”
Kala-azar is called a silent killer because its early warning signs, like fever, fatigue, weight loss, and lack of appetite, can be easy to dismiss. But if untreated, the neglected tropical disease is deadly in 90% of cases. It is caused by Leishmania parasites transmitted through the bites of sandflies, which thrive in sandy environments such as anthills and Acacia forests. These tiny insects are most active at night, which makes them particularly dangerous for pastoralists, whose work raising goats and sheep requires them to be outdoors in the evenings.
An ant hill near a home in Loima, Turkana on December 12, 2024; people living in a home so close to an ant hill are at increased risk of kala azar. Scovian Lillian
Recurrent kala-azar outbreaks have ravaged arid Turkana County, ~700 kilometers (435 miles) from Nairobi in northwestern Kenya. Reported cases have grown steadily from 157 cases in 2018 to 432 in 2020. Last year, 200+ cases were treated, but the disease’s high death rate remains a major challenge. (Data on kala-azar deaths in Turkana in 2024 are not yet publicly available.)
Kennedy Wasilwa, an LCRH clinical officer, says that kala-azar cases have surged since July. The hospital now diagnoses and treats around five to 10 cases per day, a significant increase from previous years. In December, more than 50 children were being treated for kala-azar at the LCRH.
Many patients are referred from health care facilities that have less capacity to diagnose or treat the disease. “Patients often arrive here with advanced cases,” Wasilwa says. “Some come in with severe anemia, others with TB, pneumonia, or even HIV. Treatment is possible, but patients need to be stabilized before we proceed.”
As the Leishmania parasites invade the body, they hide inside immune cells, weakening the body's defenses, causing inflammation, and damaging organs like the spleen, liver, and bone marrow. An estimated 50,000 to 90,000 new cases of kala-azar occur worldwide each year, most of which go unreported, according to the WHO. The disease continues to be a major health problem in the Americas, East Africa, North Africa, and West and South-East Asia. Four countries—Kenya, Brazil, Ethiopia, and Sudan—represent 60% of global cases. In Kenya, kala-azar is endemic in Baringo, West Pokot, Isiolo, Marsabit, Mandera, and Wajir counties as well as Turkana County.
A 2023 Drugs for Neglected Diseases initiative (DNDi) report outlines the need for safer, simpler alternatives to the current standard treatment for kala-azar in Eastern Africa—especially for children, who comprise up to 70% of cases. [Ed. Note: Journalist Scovian Lillian received a DNDi media fellowship for Eastern African health journalists that supported reporting for this story. DNDi did not edit or approve the article.] Improving awareness of the miltefosine and paromomycin (MF+PM) treatment option is crucial for combating kala-azar in the region and providing better care to the most vulnerable, per the report.
In 2010, the WHO recommended a 17-day treatment regimen to reduce hospitalization, replacing the earlier 30-day standard (two daily injections and oral drug). The WHO is about to recommend a new regimen—a combination of a daily intramuscular injection and an oral drug regimen given daily for 14 days—to reduce hospitalization and the number of injections.
In Turkana County, treatment primarily follows Ministry of Health guidelines, which include a first-line treatment regimen sodium stibogluconate and paromomycin, administered intramuscularly over 17 days. The treatment costs roughly KES30,000 ($234) per patient, though it can vary based on the specific regimen, hospitalization duration, and health facility.
When 8-year-old Esekon Nangiro fell ill in August, he had malaria-like symptoms. His father, Nangiro Loyopo, gave him over-the-counter medications and herbal medicines. The boy did not improve, however, and he began coughing and experiencing chest pains. His father, a pastoralist, stopped working so he could stay in the hospital with his son.
Eight-year-old Esekon Nangiro sits with his father, Nangiro Leyopo, and other parents of kala-azar patients outside the LCRH treatment facility on December 10, 2024. Scovian Lillian
“We have seven days left to complete the treatment and be discharged so that I can go look after my other children and my goats. This sickness is bad, I see other children with swellings around the tummy,” Loyopo says. “When we leave here we shall sleep in mosquito nets to prevent further harm [from sandfly bites].”
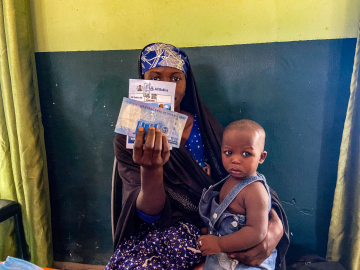
Prevention methods, which include insecticide-treated nets and raising awareness about kala-azar transmission, are critical, says Cherinet Adera, a senior market access manager at DNDi Nairobi. “Children are the most vulnerable to kala-azar because of their immune system and malnutrition,” Adera says. “Adults who spend time outdoors at night are at greater risk, so public education is vital.”
The county government, in collaboration with health partners, has launched outreach programs, and there are ongoing efforts to improve diagnostic tools and reduce misdiagnoses. Kenya’s Ministry of Health, alongside partners, is implementing a strategy to eliminate kala-azar as a public health issue by 2030. This includes deploying improved diagnostic tools, mapping disease prevalence more accurately, and enhancing public health education to reduce misdiagnosis.
Additionally, WHO and Eastern African countries launched a framework last June to eliminate kala-azar—emphasizing early diagnosis, treatment within 30 days, vector control, effective surveillance, and integration of HIV treatment for co-infected patients. The goal is a 90% reduction in cases and the elimination of child deaths from the disease by 2030.
Bangladesh’s 2023 success in eliminating kala-azar proves that such ambitious goals are attainable. “Although there is no region in Africa that has eliminated it, we are hopeful to get there by 2030 through collaboration and research,” Adera says.
Health workers, caregivers, and communities alike are coming together to fight kala-azar, hoping that improved treatments, preventive measures like insecticide-treated nets, and continued public education will erase the disease’s threat to Turkana County.
For now, the fight continues, one child at a time.
Scovian Lillian is an independent journalist focused on science and health in Nairobi, Kenya. She worked on this story as a recipient of the DNDi media fellowship for Eastern African health journalists.
Ed. Note: The reference to the WHO treatment regimen was updated on January 16, 2025 to clarify that the WHO is expected to recommend a new regimen—a combination of a daily intramuscular injection and an oral drug regimen given daily for 14 days—soon.
This article is part of Global Health NOW’s Local Reporting Initiative, made possible through the generous support of loyal GHN readers.
Join the 50,000+ subscribers in 170+ countries who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues.
Kennedy Wasilwa, an LCRH clinical officer, attends to a kala azar client at LCRH. December 10, 2024. Scovian Lillian