Digital Health Tools Are Too Slow and Too Hard to Use
A nurse in northern Bangladesh sees more than 100 patients before her clinic closes its doors for the day. From 8 a.m. until early afternoon, she consults with patients, takes blood pressure measures, administers medications, and, finally, records their data. On average, clinicians in Bangladesh see a new patient every two minutes. This scene is typical in many countries.
Even in the U.S., where a care team typically has more than 15 minutes per patient, health providers’ top complaint about electronic health records is that they take too much of their precious time and detract from patient interactions. As Richard Wachter, MD writes in The Digital Doctor: Hope, Hype, and Harm at the Dawn of Medicine’s Computer Age, “While someday the computerization of medicine will surely be that long-awaited ‘disruptive innovation,’ today it’s often just plain disruptive: of the doctor-patient relationship, of clinicians’ professional interactions and workflow, and of the way we measure and try to improve things.”
The bottom line: Digital health software is too slow and too hard to use. We must make user-centered software that is fast and easy for health care workers to utilize if we want to strengthen health programs and improve patient outcomes.
Those who design software are often too far removed from the problems on the ground. Bureaucrats and software developers (like me) typically sit in offices in large cities, far away from health care workers in busy clinics and community health workers going door-to-door to treat patients. From our offices, it’s easy to conjure up extra data fields that sound useful but will ultimately burden health care workers with data entry. The only way to make software that health care workers love using is by regularly testing software in the field with real users in their real-world work environments.
It’s possible to make software that respects clinicians’ precious time. Our team developed a tool for managing millions of patients with chronic disease, called Simple, which takes health care workers only 13 seconds to enter each patient’s data. Monthly reports that used to take two to three hours to develop are auto generated. We found that health care workers save on average 24 minutes a day versus paper records—time that can be used to deliver better patient care.
You don’t need to be Google to do user-centered design. The user-centered design process to create this type of success isn’t rocket science and can be replicated by many digital health teams if they agree to a set of core actions critical for success:
- Make it explicit that speed and usability are critical. Observe health care workers and aim to reduce data entry to a reasonable percentage of each patient visit. We knew health care workers in Bangladesh had two minutes per patient, so we aimed for under 20 seconds for data entry—a goal placed in bold for the whole team to see, so it was a key driver for our product requirements, engineering, and design.
- Radically reduce data fields. We worked with health workers and program managers to select the bare minimum of data necessary for good clinical care and for reporting indicators to drive program success. Too many health programs aim to collect comprehensive data, which burdens health workers and often reduces data quality. It’s tough to choose not to collect data, but it’s the crux of a performant digital system.
- Most importantly, watch health care workers use your tool and improve it iteratively based on observations and user feedback. We did more than 60 user testing sessions—pinpointing where health care workers found digital forms confusing and refining and testing them until we got it right.
We recently published a free practical guidebook for developers and health program managers interested in developing efficient digital systems for busy clinical environments, drawing on these principles.
I hope we can all agree that clinicians deserve to spend quality time with their patients and not with their eyes glued to a screen. By committing to develop high performance and easy-to-use software, we can finally deliver on the promises of digital health that improves patients’ health.
Daniel Burka is the director of design for the digital team at Resolve to Save Lives. He was previously a design partner at Google Ventures and spent a decade leading design at startups in Silicon Valley.
Join the 50,000+ subscribers in 170+ countries who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share this link with friends and colleagues.
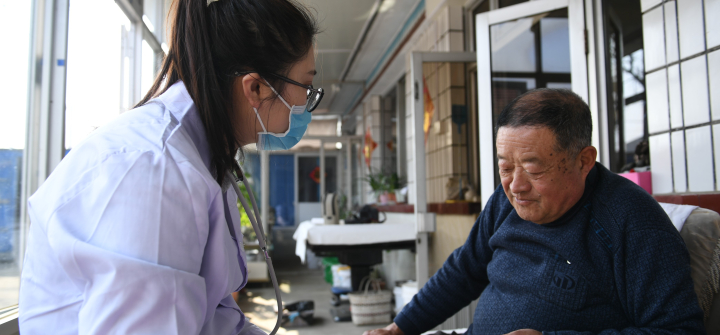
Sun Yi, a village doctor, helps a villager register health information at Qianyang Village, Donggang City, China. April 6, 2021., Cai Xiangxin/Xinhua via Getty