Socialized for Scarcity: Surgical Care in Tanzania’s Remote Refugee Camps
Peau d’orange. French for “skin of an orange,” the term refers to a specific physical exam finding of breast tissue that is swollen, tough, and red—usually because of cancer.
That is exactly what came to mind on May 18, 2023, when we were asked to examine a 40-year-old Tanzanian woman who had just arrived at Nyarugusu refugee camp’s main health post. We were in Western Tanzania volunteering clinically as part of a longstanding collaboration with the Tanzanian Red Cross Society (TRCS), which oversees health services for the 28-year-old refugee camp that is home to nearly 150,000 Congolese and Burundians seeking refuge from violence in their home countries.
Our patient Afia,* did not look well. Unable to sit up because she was so short of breath, she was placed on a cot where her condition continued to worsen before our eyes. Sweating profusely, she was in respiratory distress and had very high blood pressure with a low blood oxygen level. On exam, her left breast was hard and leathery, surrounded by chains of swollen lymph nodes under her skin like grapes on a vine.
We quickly realized how dire the situation was. There were many potential causes of Afia’s acutely unstable vital signs, and it was unlikely that we would be able to successfully identify and reverse the underlying problem, given the camp’s limited resources. We worried that without prompt diagnostics and intensive care, Afia was unlikely to survive. Unfortunately, we were correct. Within 30 minutes of her arrival, Afia’s heart stopped beating. What followed was a genuine but improbable attempt at resuscitation—a bridge to nowhere.
Why? Despite giving every therapeutic we had on hand, she arrived in critical condition and many of the medications she needed were not available. The camp’s single bag-valve mask to support her breathing was borrowed from a patient undergoing surgery in the operating theatre. Even if we had succeeded in stabilizing Afia, the nearest intensive care unit was hours away and transporting such a critically ill patient would be near impossible.
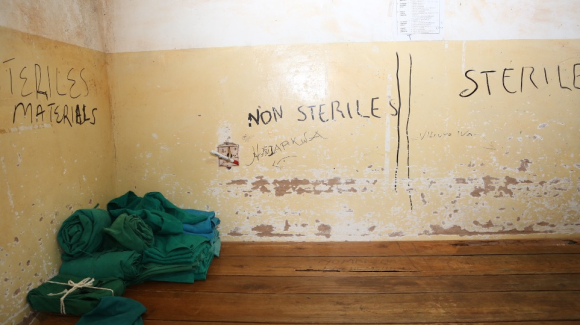
Surgical supplies stacked in a corner of a room Nyarugusu refugee camp’s operating theatre. Zachary Obinna Enumah
That Afia was a Tanzanian citizen seeking health care in a refugee camp reflects a truism across much of the world: Many camps exist in clinical deserts—geographically remote areas with little health infrastructure where local populations are often impoverished and underserved. In the communities surrounding Nyarugusu in Western Tanzania, poor access and unaffordability push many to bring their loved ones to the refugee camp, where they know they will not be turned away or charged exorbitant fees for surgery or medical care.
What patients may not fully appreciate is that the camp’s medical facilities are dramatically under-resourced. Despite existing for more than 25 years, Nyarugusu still lacks reliable electricity. The main hospital relies on a diesel-powered generator to keep the lights on during emergency surgery. There is no X-ray machine, most of the laboratory equipment is non-functional, and essential medications are often out of stock. There is only one functioning ventilator machine and not a single defibrillator in camp for emergency resuscitation. Chronic staffing shortages have grown more acute as budgets are cut each year; TRCS’ funding from UNHCR has been cut by 63% since 2020 as global attention has turned to Gaza and Ukraine.
We do not seek to minimize or undermine the tremendous humanitarian needs in places like Gaza and Ukraine, but rather to highlight the counterintuitive lack of progress in chronic refugee settings and the tangible impacts of budget cuts.
The ongoing suffering in places like Nyarugusu represents the human cost of a broken global humanitarian aid system. In a world that often perceives refugee populations as economic liabilities rather than assets, grossly excessive morbidity and mortality is treated as an acceptable norm, one that remains largely unseen and unaddressed.

A UNHCR tent in Nyarugusu refugee camp. Zachary Obinna Enumah
In settings with such dramatic resource constraints, investment in essential surgical care for conditions such as breast cancer is often dismissed as “not cost-effective.” Of course, it is highly cost-effective (for some) to not provide care to impoverished people living in underserved communities. But there is a cost. It is borne, often silently, by the families of those who suffer and die from untreated disease—as well as the societies in which they live. This is as true in urban America as it is in rural Tanzania.
In places like Nyarugusu, untreated does not mean undiagnosed. Hundreds of refugees who have sought care inside the camp have conditions meriting further workup or treatment but face lengthy waitlists to receive referrals for care outside the camp. Because their conditions are deemed stable their cases are deferred, often for months or years—but over time, these problems can become life-threatening emergencies.

The post-op ward in Nyarugusu refugee camp's health center. Zachary Obinna Enumah
As we drew a shawl over Afia’s lifeless face, her sister-in-law wept. We tried to offer consolation, feeling upset but not surprised by what seemed like an inevitable outcome. That we perceived her death as unavoidable reflects our own socialization for scarcity. Elementary investments in basic diagnostics such as X-ray and point-of-care ultrasound could free up valuable referral resources for patients like Afia, whose cancer may have been curable if treated at an earlier stage.
As the global count of refugees and displaced people climbs into the hundreds of millions, there is a natural inclination to disengage. The numbers are too overwhelming; the need is too great. Incremental solutions are often decried as unsustainable—or worse yet, unjust. While we may not be able to help every refugee or displaced person, we cannot lose the capacity for hope—to care enough to try.
*Name changed to protect patient privacy.
Alexander J. Blum, MD, MPH, is an internal medicine resident in the Hiatt Global Health Equity Residency at Brigham and Women’s Hospital in Boston, Massachusetts. His work focuses primarily on refugee health and human rights, systems strengthening, and neglected tropical diseases in South Asia and East Africa.
Zachary Obinna Enumah, MD, PhD, MA, is a surgical resident at Johns Hopkins Hospital in Baltimore, Maryland. His research focuses on quantitatively and qualitatively assessing the burden of surgical disease in refugee settings. His collaborations in Tanzania span more than a decade.
Join the 50,000+ subscribers in 170+ countries who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues: https://www.globalhealthnow.org/subscribe.
The surgery building in Nyarugusu refugee camp’s main health post on April 11, 2022. Alexander J. Blum






