Psychiatry in Sierra Leone, Part I: Inside the Movement to Transform Mental Health
This is the first story in a 2-part series. See also Part II, The Movement to Change the Narrative, published on Friday, May 17, 2024.
FREETOWN, Sierra Leone—“Look!” a young, exasperated mother exclaims, “Look at his feet!”
A hush falls over the hospital intake room as patients and triage nurses alike glance toward Ishmael. Holding his mother’s shaking hand, he is led to a small scale in the center of the triage where his cuffed jeans reveal bloated feet, covered from the shin down in mottled skin and scars. These look nothing like the feet of a young man in his 20s, more closely resembling the swollen limbs of a heart failure patient.
“His heart is being affected! And still, he goes back to smoke!” she says.
Hearing his mother’s voice tremble with desperate confusion, Ishmael bows his head and silently follows a nurse to the consultation room of Abdul Jalloh, MD, of the Sierra Leone Psychiatric Hospital (SLPH). Jalloh is one of a handful of consultant psychiatrists at the hospital helping to battle an unprecedented addiction crisis enveloping the country’s youth involving kush—a synthetic cannabis blend, purportedly adulterated with such toxic substances as formalin, insecticides, and even human bones.
Several years ago, Jalloh was one of only three psychiatrists in the country, but now he is aided by a team of seven young trainees. They’re part of a new psychiatry residency program, accredited in 2022—the first in Sierra Leone’s history.
Jusu Mattia, MD, is the medical superintendent of SLPH and was the first psychiatry trainee in the SLPH residency program, which he has seen evolve from a fledgling dream to an ever-expanding treatment program. Today, the facility is equipped with 150 beds, a child-adolescent unit, occupational therapy, recreational facilities, and green spaces. More recent innovations, such as the construction of new wards dedicated to substance use, have made SLPH a mecca for patients like Ishmael.
With a burgeoning need and limited resources, the task is an enormous challenge. “Substance use disorders are the biggest psychiatric problem that we have … it’s the majority of patients we see,” Mattia explains.
Addressing the Mental Health Crisis in Sierra Leone: Challenges
Back in the waiting room, the chairs vacated by Ishmael and his mother are quickly filled by other patients seeking treatment—some of them with telltale swollen feet, a sign of kush addiction. They will join the estimated 90% of patients at SLPH being treated for addiction to kush—a potent drug that is as addictive as it is harmful.
“The addictive potential is so high that you don’t need to be taking it for a long while for you to become addicted,” says Mattia. “You just need probably one or two puffs. You’ll keep using it forever if you are not checked.”
A new treatment ward, built to accommodate the heavy influx of substance use disorder patients at SLPH in Freetown, Sierra Leone. September 2023. Image: Blessed Sheriff
Beyond its physical effects, the societal impact of the drug has been felt nationwide. As Kelfa Koromba-Kpallu, MD, (SLPH’s chief resident) observed, “It doesn’t have barriers. It affects those who are middle-income, university students, graduates, working-class people … it’s affecting every sector of our community.” No matter one’s socioeconomic background, kush addiction can be financially devastating because it is a relatively expensive street drug, selling for 5–7 leones (less than $1)—almost triple the cost of marijuana in Sierra Leone. Additionally, addictions can begin startlingly young, according to Haja Abibatu Jalloh, MD, (henceforth referred to as Abibatu Jalloh as distinguished from Abdul Jalloh— no relation), a resident who helps run the child psychiatry service at the hospital: “Some kids, they will tell you they started using drugs when they were in primary school.”
But kush isn’t the only mental health crisis faced by the country. SLPH commonly treats patients with epilepsy, psychotic disorders, developmental disabilities, dementia, and other psychiatric conditions historically neglected by the medical system. However, limitations in workforce capacity and training have made these mental health issues difficult to navigate.
As the only psychiatric hospital in the country, SLPH contends with the daunting burden of mental health care for a country of 8 million people. Just 10 psychiatrists now work there, including the seven new trainees—many of whom found themselves here against all odds. Mattia himself originally had no plans to become a psychiatrist: “To be very honest with you, it never crossed my mind.”
For most of the residents, working at SLPH was their first real exposure to the mental health field. “In medical school, we don’t do much psychiatry. Just the basics,” says Abibatu Jalloh. In her recollection, the psychology curriculum at the College of Medicine and Allied Health Sciences, Sierra Leone’s only medical school, was “a whole new thing” for the seven students who eventually became Sierra Leone’s first domestically trained psychiatrists. Compounding this fact is the reality that for many years, SLPH “was not really a place anybody would like to be,” according to Koromba-Kpallu. Abibatu Jalloh agrees, stating, “It was scary. If you had come here six years ago, you would not enter this facility.”
In the past, labyrinthine walkways and dark isolating wards made SLPH a much more intimidating facility—for both medical students and the public at large. The cries of patients echoed off the hospital’s high walls and spilled into the surrounding communities. With such a frightening façade, it was no wonder that mental illness and those who treated mental health conditions were heavily stigmatized. Abibatu Jalloh remembers running out of the examination room after completing her primary exams for psychiatry, attempting to avoid contemptuous questions from classmates: “People stigmatize you. Sometimes they even look at you as if you have a personality problem … and these are our colleagues, not to speak of the general population!”
Haja Abibatu Jalloh at one of SLPH's newly renovated outdoor recreational facilities in Freetown, Sierra Leone in September 2023. Image: Blessed Sheriff
In fact, a flood of new investments and infrastructural renovations at SLPH (totaling about $2.5 million, jointly funded by Partners in Health and the Ministry of Health) have completely revolutionized Sierra Leone’s educational environment for psychiatry. These innovations have transformed the once infamous hospital to a modern facility with bright and lush landscaping, recreational facilities, and unprecedented access to mental health care including free medications and a cadre of dedicated support staff comprised of occupational therapists, a clinical psychologist, nurses, and social workers. Among the newest renovations: a child and adolescent mental health facility, staffed primarily by two psychiatry residents, Abibatu Jalloh and Elizabeth Allieu, MD. The renovations were so drastic that, at first, locals in the surrounding communities thought it was a different hospital entirely.
These changes have spurred a surge of interest in services for mental health: “Now we have infrastructure. We have drugs. People are seeing results. That is why we have so many patients. When I came here at first, sometimes you’d hardly see one patient. But now, everyone is talking about mental health, so people come,” says Abibatu Jalloh.
Blessed Sheriff, MPH, a fourth year medical student at the Warren Alpert Medical School of Brown University and recent graduate of the Johns Hopkins University Bloomberg School of Public Health, traveled to Sierra Leone with support from the Johns Hopkins-Pulitzer Global Health Reporting Fellowship in 2023 to report on efforts to transform mental health care in the country, including a psychiatric hospital’s innovative treatment methods and the first class of psychiatry residents trained there.
Join the 50,000+ subscribers in 170+ countries who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues.
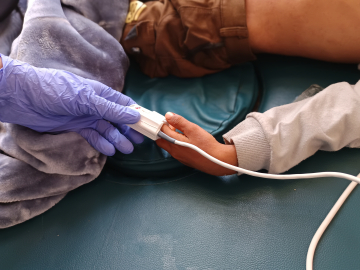
The pediatric ward of the Sierra Leone Psychiatric Hospital in Freetown, Sierra Leone. Image; Blessed Sheriff.