Psychiatry in Sierra Leone, Part II: The Movement to Change the Narrative
This is the second story in a 2-part series. Part I, Inside the Movement to Transform Mental Health in Sierra Leone, was published on May 15, 2024.
FREETOWN, Sierra Leone—Among Sierra Leoneans, there is a steadily growing movement to change the narrative around mental health. Medical students now have enhanced exposure to psychiatry, with two required rotations at the Sierra Leone Psychiatric Hospital (SLPH) throughout medical school. Jusu Mattia, MD, the medical superintendent of SLPH, states that such educational opportunities would have made him a better psychiatrist and more aware of the complex needs of his patients during training.
Medical trainees are also changing their perception of psychiatry, as it is revealed to be a promising and fulfilling profession—one where you can make an obvious difference. “The work is tense,” admits Mattia, “but you go home satisfied that you have seen a patient, and the patient goes back well … these are some of the things that keep us going.” Meaningful mentorship from the three senior consultant psychiatrists helping to lead the residency program also played a large role in changing the narrative.
Kelfa Koromba-Kpallu, MD, a resident at SLPH, recalls when Edward Nahim, MD, then a psychiatry consultant, gave lectures at his medical school class: “He made the environment so relaxing, that was the most comfortable period I ever had in my whole medical school experience. I said straightaway, ‘Okay, I will do psychiatry. I like it.’”
Mattia recalls as well how the consultants guided him and other students into psychiatry: “My interactions with the psychiatry consultants – like George Eze, MD– actually changed a lot of my perspective. Thank God we met with the right people and they’ve oriented our minds to the future; psychiatry is a great area. We started giving in slowly, and today this is one of the best hospitals that you can work in as a medical doctor.”
With a newly cultivated passion for mental health, Haja Abibatu Jalloh, MD, described how she and her fellow residents regularly forgo leave time to assist their fellow colleagues with heavy patient loads and even, at times, contribute their own salaries to patient care. All the while they endure pervasive misconceptions about the hospital and what they do. “We are branded as being crazy because we are associated with this hospital,” says Mattia, “but we are able to withstand the stresses of stigmatization and that is something to be proud of.”
Mental health awareness is chipping away at the societal stigma against mental illness in Sierra Leone. In the past, many mentally ill patients were abandoned at SLPH and chained in hospital wards too under- resourced to meet their needs. Back then, the hospital was colloquially known as the Kissy Crase Yard (the Kissy Crazy Yard) and avoided by locals and doctors alike. Today, most citizens still refer to SLPH as the Crase Yard, but some of the stigma associated with receiving treatment there has fallen away. “We have gained a lot in the last four years. Before I came here, they didn’t bring patients here. The hospital, the view of psychiatry, and mental health nationwide is changing rapidly. People are seeking help now and this is the only hospital we have that can take care of them,” says Koromba-Kpallu.
What kind of patients come to SLPH for help? Though information about specific mental health disorders and their prevalence in the country are largely unavailable, the WHO estimates that more than one in five people are likely to have a mental health condition in LMICs like Sierra Leone. According to Mattia, the vast majority of SLPH’s patient caseload consists of young men addicted to kush, a synthetic adulterated cannabis blend. The use of kush has become an epidemic, straining an already fragile health system.
Despite these workforce constraints, Koromba-Kpallu describes a compassionate system of addiction care for kush patients: “We take a history of the patients, identify their strengths and weaknesses, and start kush detoxification,” a process that can be made especially painful by the withdrawal effects of the drug, including tactile hallucinations, agitation, insomnia, and anorexia. However, medications such as anxiolytics can ease the detoxification process. “And then,” Koromba-Kpallu continues, “We teach them how to live without kush. Give them refusal skills and change their perception of the drug.”
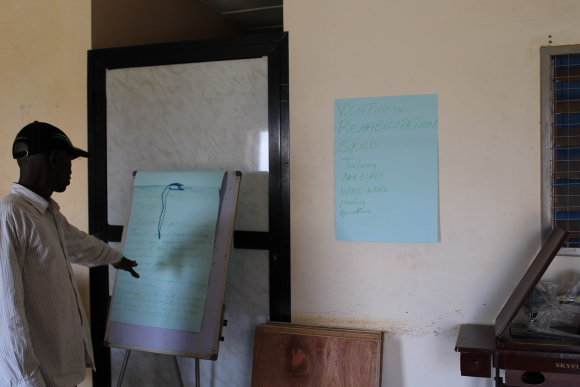
An occupational therapist at SLPH discusses skills training. Image: Blessed Sheriff
Part of this stage involves family therapy, to help parents like Ishmael’s mom understand how to support long-term recovery for their loved ones outside of the hospital. Finally, patients are reintegrated into their communities with the help of social workers and occupational therapists who provide skills-training and support with educational expenses. Partners in Health provides essential financial assistance in the reintegration process, Mattia reports: “Some patients don’t have rooms, so they rent houses for them. They give them school fees and encourage them to go back to school. Some others are given money to start working in different vocations.”
The Mental Health Coalition, a decade-old grassroots organization, is another key partner in supporting the reintegration of mental health patients back into the community. Their advocacy efforts have drawn national attention to the plight of those disabled by mental illness, and they host awareness campaigns and interventions in seven districts across the country—helping to advance the mental health movement beyond SLPH. “Systems are being put in place to make sure that mental health issues, conditions, and other disabilities are being taken care of,” says Joseph Myuma, MHC’s assistant program manager and head of communications, advocacy, and networking. He adds: “It’s rare to go into a community where people don’t talk about mental health issues now.” The motivation for mental health promotion, particularly amid the kush crisis, is clear: “For us Africans, our children are our greatest investment, and nobody wants to do bad business.”

Founders of the Mental Health Coalition – Sierra Leone. Image: Blessed Sheriff
Looking Ahead: Next Steps and Limitations
However clear the motivations are for the mental health movement in Sierra Leone, its limitations are obvious as well. Resources have not expanded rapidly enough to accommodate the many patients nationwide who seek help. For a country of nearly 8 million people, SLPH employs less than 1 psychiatrist per 100,000 persons. This figure is well below average for the African region. Sierra Leone would need to multiply its mental health workforce five times over to match that of its neighboring west African country Senegal, and over 200X to match the density of the mental health workforce in high income countries like the U.S.
“This is the only referral hospital we’ve got for the whole country. Some people leave their villages from the provinces to come all the way to Freetown for treatment,” explains Sao Fatorma, a new resident at SLPH. “And, of course there is no funding,” adds Mattia. “If you look at the human resources for mental health service delivery across the country, it’s really appalling.”
There is no primary level of care for mental health in Sierra Leone, forcing SLPH to treat a wide spectrum of needs rather than focusing on severely ill patients like most specialty hospitals. In order to create a primary level of care, Fatorma believes that the country would need to give greater attention to secondary training and the establishment of new treatment centers across the country. But for now, he says he is unsure if such treatment centers are even on the list of priorities for politicians. Mattia shares the same sentiment, adding that “mental health is usually forgotten about” at the ministry level of government.
With a lack of political and institutional support, Mattia fears that some gains in mental health training might be lost in the near future: “If you randomly ask 10 medical students what their plan is, it is very likely you are not going to get one person who will tell you they want to do psychiatry … for this program to be revamped and sustained, some attention needs to be paid to the specialty. Otherwise, I’m afraid we might just be the last set of people doing psychiatry here.”
Still, Koromba-Kpallu believes that the same kind of mentorship that sparked his initial interest in psychiatry will attract new trainees: “Most of us were attracted to psychiatry by other people in the field … it’s about our experience here; that is what is going to make people come here.” Like many of his colleagues, Koromba-Kpallu intends to become a mentor for others. He hopes that “by the end of residency I will be a good teacher … that’s what I really want. We will be training the future psychiatrists.”
Resident Haja Abibatu Jalloh, MD, is of similar mind, stating “once I finish residency, I’d want to become a fellow—a consultant,” like those currently helping to run the psychiatry residency program. As one of the youngest residents in the program, Fatorma is excited about the possibility of a growing workforce in mental health. He hopes that after training, residents will not limit themselves to SLPH. “The rest of the country is waiting for our services.”
Blessed Sheriff, MPH, a fourth year medical student at the Warren Alpert Medical School of Brown University and recent graduate of the Johns Hopkins University Bloomberg School of Public Health, traveled to Sierra Leone with support from the Johns Hopkins-Pulitzer Global Health Reporting Fellowship in 2023 to report on efforts to transform mental health care in the country, including a psychiatric hospital’s innovative treatment methods and the first class of psychiatry residents trained there.
Join the 50,000+ subscribers in 170+ countries who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues.
View of Freetown, Sierra Leone. Image: Blessed Sheriff





