Amsterdam’s Struggle to Improve Sex Worker Health
AMSTERDAM, Netherlands—Any given weekday, a dozen or so patients shuffle through a small clinic retrofitted in one of Amsterdam’s iconic rowhouses. Once inside, they’re confronted with all the essentials of a standard medical office: a no-frills check-in desk, a tidy waiting area with a not-so-tidy stack of magazines, and a small back room with a gynecological exam chair and an intimidating display of metal instruments.
The only real clues that this isn’t just any health clinic are the oversize vintage ad for vaginal lubricant, in which a woman slides effortlessly down a stair railing, and the decorative 3D shadow boxes featuring, for example, a man in a jungle-themed bedroom stroking a strategically placed blow-up palm tree.
This is the Amsterdam Center for Sex Workers (ACS), a government-funded clinic that caters to the region’s 5,000 to 7,000 sex workers, including those who offer their services in the iconic window workspaces of De Wallen—the most prominent of the city’s three red light districts. It also provides care for those working as escorts, in sex clubs, massage parlors, online, or from home. The clinic is at the center of local efforts to improve health care for sex workers—and while it has become more accessible since the Netherlands legalized prostitution in 2000, the Dutch approach is far from seamless.
A web of immigration and labor policies, logistical hurdles, and social stigma mean some sex workers are unable to access the health care system. Sex workers who don’t have the right work permit and those under 18 (21 in Amsterdam) all work illegally and may experience worse working conditions, greater risk of exploitation, and have difficulty accessing health care.

The Amsterdam Center for Sex Workers (ACS). Gabriela Galvin
Violet’s Story
Violet*, a sex worker from the U.K. who also works at the city’s Prostitution Information Center,lives and works in the Netherlands legally, but bureaucratic barriers made it difficult for her to get insurance, which she needed urgently to cover a lapsed contraceptive and medication for immune disorders. After a nine-month wait that she described as a “crisis situation,” Violet recently secured coverage.
“What I do makes it more difficult to openly talk about why it is so important for me to get access to these medications, and how that is going to impact other areas of my romantic and professional life,” Violet said. “Being honest about what you do raises more red flags and causes more issues [with health, labor, and insurance officials]. You'll see the smoke coming out of their ears when I'm trying to tell them the situation, the complexities around it, and there’s judgment there as well.”
Unlike Violet, sex workers from the European Economic Area—which includes the European Union’s 27 member states plus Iceland, Liechtenstein, and Norway—are eligible for legal, health, and social services. Typically, sex workers are independent contractors who must register with the Chamber of Commerce and get health insurance, like any other employed person.
The country’s shift toward tolerance has had some positive results. Between 2006 to 2013, the share of female sex workers in the Netherlands who had ever been tested for HIV rose from 63.7% to 85.8%, researchers found in 2015. Generally, in high-income countries where sex work has been either legalized or decriminalized, sex workers have better health outcomes, including greater awareness of health conditions and risks, according to a sweeping 2021 review in the International Journal of Environmental Research and Public Health.

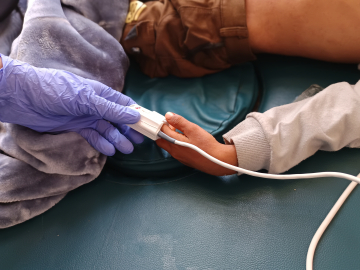
Marianne Craanen, a sexual health nurse and clinic coordinator for the Amsterdam Center for Sex Workers. Gabriela Galvin
Bridging Gaps in Care
The biggest problems today are not the availability of care itself, but rather improving access for sex workers who can be hard to reach, such as those in the unregulated sector or ethnic communities who may have their own channels for seeking care, says Lorraine Nencel, an associate professor in sociology who researches sex work at Vrije Universiteit Amsterdam.
ACS tries to bridge these gaps. The clinic does about 2,200 health consultations per year, providing free or low-cost testing for sexually transmitted infections (STIs) and pregnancy, pre-exposure prophylaxis (PrEP), hepatitis A/B vaccinations, and counseling with social workers, according to Marianne Craanen, a sexual health nurse and the clinic’s coordinator. The most commonly detected STIs are chlamydia and gonorrhea, which can be treated with antibiotics. In 2023, the STI positivity rate among female sex workers who came in for a test was 9.3%, and 29.5% among their male counterparts, Craanen said.
Yet such targeted health services can still be difficult to access. A 2020 PLOS One study identified several barriers that can stymie HIV testing for Eastern European, non-EU sex workers in Amsterdam, including wariness of Dutch health and social services, poor experiences with the health care system in their home countries, lack of knowledge around HIV risks, and low levels of Dutch or English, which is widely spoken in the city. Today, a growing share of ACS’s patients are in such “vulnerable situations,” Craanen said.
“It's so difficult to find your way in a country where you don't speak the language, where you don't know where to go, and [there are] a lot of rules,” she said. “We take a lot of time in building trust.”
That involves a lot of outreach, both online and in person, as well as coordination with partners like the Trans United Clinic. At ACS, people can typically get an appointment within three days. Patients don’t have to share any information beyond a first name; and no information is shared with outsiders, such as hospitals, nonprofits, or the authorities, without the patient’s approval. If the clinic wants to refer them to a doctor’s office—for example, to get treatment for an STI, or hormone therapy for transgender patients—the team tries to ensure speedy referrals and regular communication because, as Craanen said, “it's very easy to lose people” in the system.
ACS also has two counselors for patients struggling with their mental health, which is a key concern for sex workers around the world, according to the advocacy group European Sex Workers Rights Alliance. That’s not because the job necessarily causes mental health issues, but rather because many mental health professionals are poorly equipped to meet sex workers’ needs, according to Sabrina Sanchez, ESWA’s executive director.
“We have to face that when we seek mental health care, sometimes we find the typical therapist wants to blame everything on your sex work, for all the issues that you can have,” Sanchez said.
Moving the Red Light District
Violet noted that health challenges could be compounded if the city moves forward with a plan to uproot De Wallen’s window workers to an “erotic center” on the outskirts of town. Local policymakers say the center is needed to crack down on rowdy tourist behavior in the red light district, but sex workers have opposed the plan, saying it could make their work more dangerous by isolating them from public view, increasing competition between sex workers, and making it harder to turn down prospective clients.
The proposal is the latest in a long string of efforts to curb the red light district’s reach. From 2007 to 2018, the city closed more than 100 windows in De Wallen, prompting some sex workers to move to the unregulated sector. Currently, about 290 windows remain.
A spokesperson for the city said the erotic center would aim to “improve the human rights position of sex workers” by steering people toward the licensed sector and offering onsite health care and “necessary direct contact with the police.” Craanen said that if the erotic center opens in another area, ACS would do outreach there but keep its clinic near De Wallen.
Ultimately, sex workers and officials agree on the basics: The opening of the erotic center would not only change the red light district’s character, it would reshape the market for sex work in Amsterdam. Whether that change would significantly impact sex workers’ health outcomes and access to care is yet to be seen.
“When you impact a sex worker’s income, you impact every facet of their safety, wellbeing and health,” Violet said. “If you’re having issues with sorting out your financial situation or your household situation, your health is going to slip. It’s not going to become the most important thing.”
*Violet uses a pseudonym to protect her privacy.
Gabriela Galvin is a freelance journalist based in Aarhus and Amsterdam, originally from Washington, D.C.
Ed. Note: This article is part of Global Health NOW’s Local Reporting Initiative, made possible through the generous support of loyal GHN readers.
Join the 50,000+ subscribers in 170+ countries who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues.
A sex worker waits for clients behind her window in the red light district of Amsterdam, on December 8, 2008. Anoek De Groot/AFP via Getty