Bridging the Surgical Gap for Rural Indigenous Communities
“I have often danced the dance of life with my patients. But too often, I dance the dance of death.” —Richard Duque, social worker, Boa Vista City, Brazil
Throughout Latin America and globally, Indigenous communities face significant challenges in accessing health care, particularly when it comes to complex systems like surgical care. Whether it’s a lifesaving emergency procedure or an early-childhood intervention to prevent disability, surgical care requires an ecosystem of people, products, and processes that often fail to reach the most vulnerable people in the most remote places.
By the numbers, Brazil’s surgical health workforce appears robust. The vast majority of doctors, anesthesiologists, nurses, and other specialists, however, live in southern Brazil’s urban areas—leaving rural areas, especially in the north, without enough hospitals and workers to meet patient needs. More than six million children live more than 75 miles away from a referral center and the hope of accessible pediatric surgical care.
This inequitable distribution of the health and surgical resources and workforce is common across many countries in Latin America.
Richard Duque, a social worker and Yanomami language translator at Hospital da Crianca in Boa Vista City, is all too familiar with this reality. His hospital, located in northern Brazil’s Roraima state, is one of the region’s only treatment centers serving newborns and children. Duque sees the impact of this inequity on Indigenous children, families, and communities—and, as an Indigenous person, he has experienced these challenges firsthand.
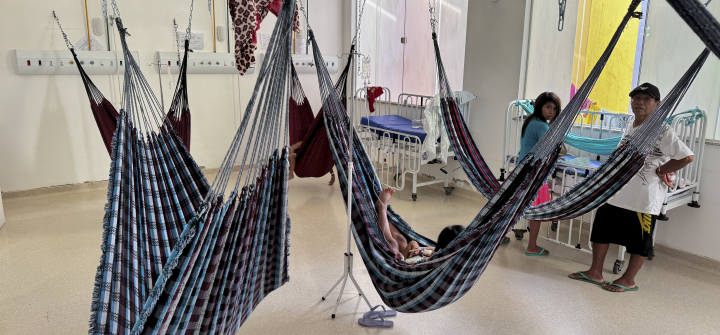
Hospital da Crianca, however, integrates the cultural traditions and needs of Indigenous people into their treatment. Indigenous people are encouraged to bring their traditional healers; meals reflect their diets at home. In their hospital rooms, hammocks hang in the place of beds. In 2020, with support from the city government, Smile Train, and the North Amazon Association for Support for People with Cleft Lip and Palate of Roraima, the hospital also became the only treatment facility in the state to offer cleft surgery and comprehensive cleft care.
Despite such pockets of progress, enduring challenges like geographic barriers, poor transportation, a lack of culturally appropriate facilities, distrust of non-traditional medicine, discrimination, and poverty mean that Indigenous peoples face unnecessary death and disability every day. Health systems and NGOs that have worked to deliver surgical care to rural Indigenous communities have learned through experience that cultural and language barriers often lead to misunderstandings and drive distrust among the populations we intend to serve—illustrating an urgent need to establish dialogues that incorporate culturally sensitive care. The neglect of vulnerable, economically challenged communities has far-reaching implications, including increased mortality, poverty, and stubborn health inequities.
But in Latin America, an opportunity to end a long legacy of neglect and exclusion for Indigenous peoples is on the horizon.
In November, Ecuador became the Latin American country to launch a National Surgical, Obstetric, Trauma, and Anesthesia Plan (commonly referred to as an “NSOAP”). But it is far from the region’s only effort to strengthen surgical systems. Through their national databases, countries including Brazil, Colombia, and Mexico are gathering crucial data on surgical indicators, while Bolivia, Haiti, Nicaragua, and other countries are reducing injury-related deaths by strengthening emergency and trauma care systems.
A Global Alliance for Surgical, Obstetric, Trauma, and Anaesthesia Care (G4 Alliance) meeting at the Smile Train Cleft Leadership Center Centrinho Bauru in Bauru, Brazil, last November further demonstrated the increasing prominence of safe surgery and anesthesia care in Latin America. Policymakers from Ecuador, Brazil, and PAHO, as well as clinicians and health workers across Brazil, addressed the state of surgical systems, challenges, financing strategies, and advocacy needs to maintain momentum.
From these discussions came a clear consensus: investments in surgical and anesthesia care throughout Latin America herald a golden opportunity for governments, civil society, communities, and the private sector to work together to narrow the alarming global gap in access to surgery and decrease the significant morbidity and mortality caused by inequitable access to safe surgical care. They must collaborate to develop and monitor surgical capacity, using agreed-upon health indicators, strengthen infrastructure and equipment available in underserved areas, and invest in training and incentivizing rural health care workers.
The complexity of surgical care necessitates a multifaceted, community-centered approach. To counter rising health care costs and growing social and income inequality, governments around the world are looking to primary health care approaches to deliver the bulk of necessary health services. These strategies must integrate surgical care, bringing essential surgical capacity closer to the entire population—with special emphasis on hard-to-reach areas and populations. Involving Indigenous, rural communities in the design of surgical care delivery programs is both a best practice from a primary health care and health systems planning perspective and an absolute necessity for people living in those communities.
Together, we can ensure every Latin American country has a clear view of its national surgical system, and a roadmap to strengthen those systems and bridge the surgical care gap. The well-being of any country or region is intrinsically tied to the health of all, and neglecting a critical service for the most vulnerable undermines the primary health care foundations on which everyone relies. It is time to take action and forge a path toward health care equity that truly leaves no one behind.
Alfredo Enrique Borrero Vega, MD, is the former Vice President of Ecuador (2021-2023) and the founder and president of the Latin American Health Consortium.
Susannah Schaefer is president and CEO of Smile Train.
Natalie Sheneman is the advocacy manager for the G4 Alliance.
Join the 50,000+ subscribers in 170+ countries who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues.
Yanomami Indigenous people inside a ward at the Santo Antonio Children's Hospital in Boa Vista, Roraima state, Brazil. January 17, 2024. Alan Chaves/AFP via Getty