Ending TB Will Cost Billions—Not Ending it Will Cost Trillions
WHO’s latest tuberculosis report painted a bleak picture—showing that TB incidence and mortality rose for the first time in almost 2 decades,.
10–11 million people developed TB in 2021, and 1.6 million of them died from the disease. Perpetually inadequate funding remains the most important barrier to stamping out the disease, which is preventable and curable but can be lethal if left untreated. In 2018, countries pledged $15 billion annually, but in 2021 just $5.4 billion was available.
How can wealthy countries help? While TB is widely regarded as a disease of poverty, G20 nations, representing the world’s largest economies, account for nearly half of all TB infections. That puts them in the strongest position to lead the fight to stamp out the disease, according to the bloc’s first-ever call to action on TB ahead of the G20 Summit this week.
High-burden countries at the helm: It’s perhaps no coincidence that Indonesia—the 2022 G20 presidency and a high burden of TB—led that call. Another high TB burden country—India—will take the reins next year.
These countries’ leadership is a promising sign for the TB fight, but there are enormous hurdles to overcome, says Suvanand Sahu, deputy executive director of the Stop TB Partnership. Sahu spoke with GHN about his wish list for funding TB efforts, what it will take to banish the disease by 2030—and what it will cost, for health and for economies, if that doesn’t happen.
First of all, why should we all be paying attention to TB?
This is a dire situation. On one hand, TB incidence and mortality is going up. On the other hand, funding is less than half of what is needed. It was completely inadequate—even pre-COVID.
TB is the biggest infectious cause of death, and only in recent years COVID has surpassed it in terms of number of deaths. We must remember: This is an airborne disease with drug resistant variants and if people with TB remain undetected, it is a serious issue.
There’s no doubt that the WHO report paints a troubling picture, but what can we learn from the bright spots? For example, TB preventive care for people with HIV is actually improving.
There are a few positive things in the report—that is one of them.
In 2018, a UN high level meeting set a target for expanding TB preventive therapy amongst people living with HIV. That's the only target amongst the many in that political declaration that has been achieved.
Why? Look at the funding levels. The Global Fund commits only 18% of its resources to TB. It commits half of its resources to HIV.
If you look at other external funding, you have PEPFAR for HIV; there’s no such presidential initiative for TB.
Another factor is political will. Some countries—mainly in Africa—despite the COVID pandemic, have continued to provide increased access to TB diagnosis and treatment. That means more TB cases are being reported.
Opportunities created by the COVID pandemic also probably made treatment more people-friendly and probably it's a lasting change that should remain.
WHO has called for countries to cover the costs of TB treatment, which it describes as potentially “catastrophic” for families. Why has that been so difficult to make a reality and how can it be improved?
TB is a disease that affects poor people more than the others, so even small out-of-pocket expenses can be catastrophic.
This is unacceptable because TB is not a new disease—it’s a disease that can be prevented, diagnosed, and treated to cure.
The only way to reduce these expenses is for national programs in high TB burden countries to cover those costs.
Otherwise, those who are unable to bear the cost remain untreated, and that comes with the huge consequences of untreated TB—where 1 out of 2 cases can be fatal.
As we’ve seen with COVID-19, countries that prioritized COVID-19 could scale up testing. They could scale up contact, tracing. They could do a lot of activities for airborne infection control. They could scale up vaccine rollouts.
Of course the poorer countries will need external funding. But what we are calling for is the heads of state to prioritize TB the same way they did COVID-19—and that means committing funding.
If the benefits are so clear, why has this been so difficult to achieve?
Many countries plan from a scarcity situation, so they are never able to plan ambitiously to end TB. To address that, one of STOP TB’s calls to action, outlined in our 8-year global plan to end TB by 2030, is to diversify sources of TB funding, going beyond the traditional domestic and the external funding, toward innovative financing.
For example, we have seen in India and more recently Indonesia, the World Bank and Global Fund getting together to provide a mix of grants and loans, so that the grant is incentivized.
What is the cost breakdown of ending TB by 2030?
We need a total of $250 billion to end TB by 2030, in line with the UN Sustainable Development Goals.
Our modeling shows that we have to do some aggressive things to get back on track to end TB, but it's possible if the money is available.
The money up front is enormous–but what is the cost of not investing in ending TB?
$1 invested in TB will get a return of $40. It has always been consistently shown that TB funding offers a strong return on investment.
We also did another analysis which looks at the cost of inaction.
If the money isn’t made available now, the economic losses, direct and indirect, will be more than $1 trillion.
Why is the G20 now uniquely positioned to prioritize TB?
50% of the TB burden is in G20 countries—but G20s are also driving the global economy. So they have the capacity to take care of their TB fight.
But also they have the capacity to do public good for other countries— to research new tools that are required for TB, like a new and effective vaccine to be able to end TB by 2030.
High TB burden countries are presiding over G20, and making it a priority. So currently the stars are aligned in the G20 agenda to take action on TB in a way that has never happened in the past.
This interview has been edited for length and clarity.
Join the 50,000+ subscribers in 170+ countries who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues.
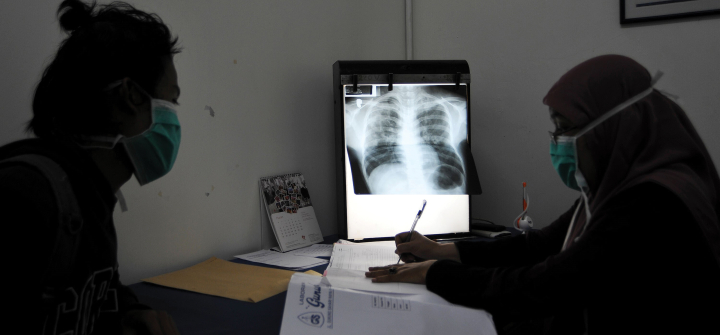
Doctor Yulismar (R) checks the condition of a tuberculosis patient at the Indonesian Association Against Tuberculosis in Jakarta, March 24, 2016. Jefri Tarigan /Anadolu Agency/Getty