COVID-19 Expert Reality Check
As the media swarms the coronavirus story, lost in the shuffle are the important public health insights about how viruses work and humans respond. To help improve understanding of the outbreak’s complex dynamics, GHN has reached out to some of the world’s most respected global health experts for their quick "reality checks" on key issues.
Subscribe to Global Health NOW's free weekday enewsletter here for more COVID-19 and public health news.
See also the Johns Hopkins Coronavirus Resource Center for more updates.
Filter Reality Check Questions
Enter a few letters on a topic to filter questions, results are displayed as you type.
Virus
-
Will a COVID-19 vaccine be as unreliable as the seasonal flu vaccine? By Kishana Taylor
-
Could SARS-CoV-2 be transmitted sexually via semen? By Jim Hotaling
-
Could air conditioning systems help spread the virus? By Ana M. Rule and Lesliam Quirós-Alcalá
-
Do we know if the virus can enter through the eye? By Alfred Sommer
-
What determines whether a virus disappears or becomes endemic? By Emily Toth Martin
-
Will most of humanity be infected by the new coronavirus? By Justin Lessler
-
How does a virus shift from zoonotic to human-to-human transmission? By David Quammen
-
Is it possible to be reinfected with the novel coronavirus? By Rachel Graham
-
How do you go about creating a vaccine against a new virus? By Peter Hotez
Outbreak
-
What are 'excess deaths' and what do they tell us? By Justin Lessler
-
Can SARS-CoV-2 be controlled, eliminated, or eradicated? By Jessica Atwell
-
What’s the worst-case scenario for this pandemic? By Laurie Garrett
-
When does an outbreak become a pandemic? By Eric Toner
-
What’s a reproductive number and what does it tell us about an outbreak’s future? By Michael Osterholm
-
What does successful risk communications look like? By Amanda McClelland
Response
-
Will COVID-19 make the coming flu season worse? By Kishana Taylor
-
What is intersectional analysis, and how could it mitigate health inequities in a pandemic? By Mireille Evagora-Campbell
-
How does contact tracing vary in different countries and cultures? By Tolbert Nyenswah
-
What does it take to be a great contact tracer? By Joann Schulte
-
Do health care workers present a risk to the community by returning home after work? By Marisa Holubar and Yvonne (Bonnie) Maldonado
-
What does “preparedness” in a country really mean? By Caitlin Rivers
-
What is the best way to counter misinformation in the media? By Amesh Adalja
-
What is it like inside a hospital biocontainment room? By Lauren Sauer
-
What’s the best way to respond to the coronavirus outbreak? By Tom Inglesby
-
Can travel restrictions and quarantines stem the spread of the coronavirus? By Jennifer B. Nuzzo
-
What are the ethical considerations of using quarantines? By Jeffrey Kahn
Minimize Your Risk
-
Do we need to worry about catching COVID-19 from toilets? By Joseph Allen
-
Can Halloween trick-or-treating be safe this year? By Amesh Adalja
-
Should I get tested if I don’t have symptoms? By Natalie Dean
-
What’s the difference between face masks and face shields? By Amesh Adalja
-
Why is diabetes considered a risk for severe COVID-19? By Ranganath Muniyappa
-
Can my kids go and play with friends? By Crystal Watson
-
What should the average person in a non-outbreak area be doing to prepare? By Michael Osterholm
-
What precautions should I take when I have to go out to get food? By Crystal Watson
-
Can the new coronavirus be transmitted via paper money? By Marilyn Roberts
Have more questions? Please send GHN any questions you'd like to see answered related to the coronavirus outbreak. Just email Dayna (dkerecm1 at jhu.edu). And, for GHN's latest coverage of the coronavirus, visit here — and, if you don't already subscribe to our free daily enewsletter, you can sign up here.
Virus
-
Will a COVID-19 vaccine be as unreliable as the seasonal flu vaccine?
COVID-19 and seasonal flu present similar symptoms, but they differ when it comes to vaccines.
Because the influenza virus evolves very rapidly, seasonal flu vaccines efficacy rates have varied (10–60% in recent years). But so far, SARS-CoV-2 has not mutated in a way that changes our reaction to the virus.
If a safe and effective COVID-19 vaccine arrives before we see a major mutation, low vaccine efficacy shouldn’t be a major issue as it is with the flu.
However, the concern with a potential vaccine for SARS-CoV-2 is that historically seasonal coronaviruses do not trigger a strong, long-lasting immune response.
So, as with the flu vaccine, we may end up needing a COVID-19 vaccine every year—but for different reasons. People get the flu vaccine every year because the virus changes. When it arrives, we may have to get a SARS-CoV-2 vaccine annually because the immunity doesn’t last.
Kishana Taylor, PhD, MS, is a postdoctoral scholar in the Department of Microbiology and Molecular Genetics at the Díaz-Muñoz Lab at the University of California, Davis, which focuses on the evolution of virus coinfection.
-
Can the bodies of COVID-19 victims transmit the virus, and what are the safest burial practices?
In general, dead bodies are not infectious and to date there is no evidence of infection via exposure to the body of a COVID-19 victim.
However, the concern is understandable given the high-profile Ebola outbreaks in recent years. Victims of that virus—and of other especially virulent diseases such as Marburg virus, Lassa fever, and cholera— are known to be highly infectious and extreme caution is necessary when burying victims.
For example, during the 2014–2016 West Africa Ebola outbreak, it was necessary to resort to cremation to protect the public from infectious bodies.
This is not necessary with COVID-19 victims. With certain precautions, it is safe to proceed with the usual burial practices based on religious and cultural traditions, while maintaining social distancing. The necessary PPE includes N95 masks, gloves, foot coverings, hair covers, eye covers—and standard hygiene practices such as frequent hand washing.
It remains important to give victims dignified burials, and families should be protected and respected throughout the burial process.
Tolbert G. Nyenswah, LLB, MPH, is a senior research associate in the Department of International Health at the Johns Hopkins Bloomberg School of Public Health. -
Could SARS-CoV-2 be transmitted sexually via semen?
COVID-19 has been found in semen—but it is unlikely to be spread that way, although it hasn’t been ruled out.
One small study of 34 Chinese men diagnosed with COVID-19 found no evidence of SARS-CoV-2 in their semen or testes ~1 month later. Another study—which didn’t address the sexual transmission question—found the virus in 6 of 38 patient semen samples. But that study involved much sicker men; the viral load by that stage could be a factor.
And, severely ill people aren’t likely having sex; that’s a bigger question during recovery.
Studies on patients with SARS-CoV-2 in their semen, testing weekly to see if and when it clears, could inform guidelines on how long post-diagnosis men should refrain from sex. Regardless, sex—impossible from a 6-foot safe distance—still isn’t a good idea for at least several weeks later, given the established risk of respiratory transmission.
Jim Hotaling, MD MS FECSM, is an associate professor of Surgery (Urology), codirector of the Fertility Integrated Practice Unit and the Surgical Population Analysis Research Core (SPARC), and director of Men’s Health at the University of Utah School of Medicine.
-
Could people who have taken antiviral drugs (such as HIV Protease Inhibitors, etc.) for many years recover faster?
Research has shown HIV protease inhibitors—drugs that interfere with a virus’s ability to replicate—block the SARS and MERS coronaviruses in lab settings. However, there is little evidence to suggest a benefit against the novel coronavirus, SARS-CoV-2, for patients already taking these drugs.
In 2003, clinical studies using HIV protease inhibitors—specifically, the FDA-approved oral combination treatment lopinavir/ritonavir—to treat SARS were associated with reduced mortality and intubation rates. However, the studies were retrospective and not controlled clinical trials.
Still, amid the desperate search to find treatments for the novel coronavirus, researchers have carried out clinical studies using these drugs on COVID-19 patients—despite the lack of published data documenting their utility against SARS-CoV-2.
Based on the data so far, there is little reason to expect patients taking HIV protease inhibitors will see a benefit against COVID-19—either to protect from infection or to speed recovery.
David Riedel, MD, MPH is an infectious disease physician at the University of Maryland where he is focused on the care and treatment of patients living with HIV.
-
Could air conditioning systems help spread the virus?
Air conditioning and ventilation are actually considered effective control strategies for reducing infection risks to the public in indoor spaces, according to a framework that occupational health professionals use called “the hierarchy of controls.”
If a ventilation system is well maintained, the risk of transmission should not be significant. By well maintained, we mean that the system is inspected periodically, the filters are changed according to manufacturer recommendations, the duct systems are cleaned periodically, and the most efficient filters available are used (for example, MERV [minimum efficiency reporting value] filters with a rating of 13 to 16 for homes; HEPA [high-efficiency particulate air] filters for hospitals). Keep in mind, that even in well-ventilated environments, people should continue following recommendations of physical distancing, face covering, and frequent hand hygiene.
At present, there is no strong evidence to suggest that a well-maintained air conditioning, ventilation, or other type of climate control system will contribute to the transmission of COVID-19.
Ana M. Rule, PhD, is an assistant professor and director of the Exposure Assessment Lab in the Department of Environmental Health and Engineering at the Johns Hopkins Bloomberg School of Public Health; and Lesliam Quirós-Alcalá, PhD, is an assistant professor in Environmental Health and Engineering at the Bloomberg School and an adjunct assistant professor at the University of Maryland’s Maryland Institute of Applied Environmental Health.
-
Do we know if the virus can enter through the eye?
There is no evidence yet that SARS-CoV-2, the virus that causes COVID-19, can gain entrance through the eye. However, there are now reports of the virus being present in tears and on the surface of the eye. While most of those patients were very ill, it is likely that the surface of the eye and its tears may contain virus and it’s best to avoid touching the eye or tears of any potential patient.
While we do not yet have any direct evidence that the virus is infectious if it touches the eye, we must assume that it is a possibility. As the general precautions all stress, anyone who touches someone who may be infected (or something they may have touched) should wash their hands immediately, and refrain from touching their own face (which would include the mouth and nose—known sites of infection—as well as the eyes).
Alfred Sommer, MD, MHS, is a professor of Ophthalmology and Epidemiology and Dean Emeritus of the Johns Hopkins Bloomberg School of Public Health.
-
What determines whether a virus disappears or becomes endemic?
Two main clues help us predict whether a virus is going to stick around. First, we consider the virus’s origins. If it came from animals and could still be circulating in animals, then no matter how good we are at getting rid of it in humans, animals could always bring it back. That’s true with influenza: Even if a certain strain disappears, a new one might emerge from animals—as we’ve seen with avian viruses.
But with a major outbreak like COVID-19 already underway in humans, the big question is how good humans are at developing immunity. And, if they gain immunity, does it stick, or does it fizzle out over time—leaving the door open a crack for the virus to return? As the first cases get further and further out from the point of infection, that data will give us a better idea of what to expect.
Emily Toth Martin, PhD, MPH, is an associate professor of epidemiology at the University of Michigan School of Public Health.
-
“What can we expect from the coronavirus circulating now? Will it change to become more lethal or more easily transmitted?”
The SARS-CoV-2 virus that causes COVID-19 will likely continue with minimal variation. It will probably stay stable because very few people are immune—so many “naïve” human hosts are still available for maintaining current transmission cycles.
This virus appears very balanced in terms of transmission-to-virulence. It also can be transmitted early in infection. Serious disease usually doesn’t occur until much later—and by that time, many patients are confined to a hospital bed. Consequently, a long transmission window is present before a person falls seriously ill, giving the virus plenty of time to spread. Selection is heavily driven by transmissibility, and the role of virulence in this process is much less clear.
Another coronavirus, MERS, has a high lethality but doesn’t transmit as easily. This one is far more virulent—and devastating. Many dangerous respiratory viruses spread efficiently before causing severe disease—and that’s what we’re seeing with SARS-CoV-2.
Ralph Baric, PhD, is a professor in the Department of Epidemiology and in the Department of Microbiology and Immunology at the University of North Carolina Gillings School of Global Public Health.
-
Will most of humanity be infected by the new coronavirus?
It is likely that eventually it will become endemic, and most of us will get infected. But one question is super important: How long will it take for that to happen? If it happens in a few months, every hospital will be overwhelmed and people will not be treated for coronavirus or other diseases. If it happens that fast, it will be an unprecedented disaster. However, if we do our best in terms of prevention by practicing social distancing, reducing travel, not going to work when we’re sick, we could slow spread of the disease. If the same 60-70% infection of the global population is spread over 3 years, then hospitals don’t get overwhelmed, people can get treated, and we have time to develop a vaccine—it’s a completely different story.The difference between it happening fast or slow is potentially the difference between a 1918 flu level event and a bad flu season level event. We have control over that.
Justin Lessler is an associate professor of Epidemiology at the Johns Hopkins Bloomberg School of Public Health.
-
How does a virus shift from zoonotic to human-to-human transmission?
When a virus passes from a nonhuman animal into a human, we call that moment of spillover a zoonotic transmission. It’s an ecological event. What happens next depends on evolutionary potential and chance. If the virus is adaptable, it may succeed in replicating and proliferating in the new human host. Maybe it kills the person and the line of transmission comes to an end there—as happens with rabies. But if the virus is even more adaptable, it may acquire the ability to pass from one human host to another, perhaps by sexual contact (as with HIV), perhaps in bodily fluids such as blood (as with Ebola), perhaps in respiratory droplets launched by coughing or sneezing (as with influenza or SARS). What makes a virus adaptable? The changeability of its genome, plus Darwinian natural selection. Those viruses with single-stranded RNA genomes, which replicate themselves inaccurately and therefore have highly changeable genomes, are among the most adaptable. Coronaviruses belong to that group.
David Quammen is the author of more than a dozen books, including Spillover: Animal Infections and the Next Human Pandemic, and hundreds of articles for publications including National Geographic, The Atlantic, Harper’s, Rolling Stone, and many others.
-
Does an overreaction by the immune system play a role in COVID-19 deaths, or are they caused strictly by damage inflicted by the virus itself?
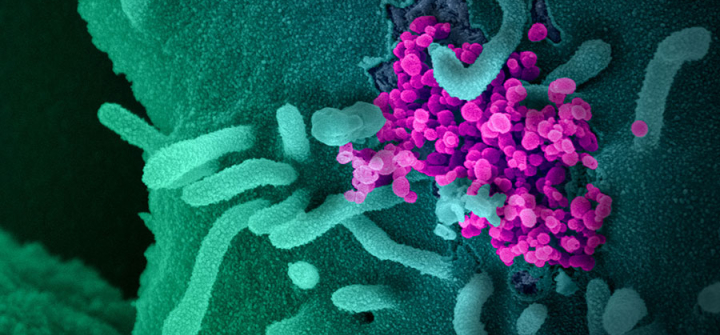
Infection with SARS-CoV-2 is associated with respiratory tissue damage that can impair lung function and even cause death. Though it is likely that both the virus and immune system contribute to this process, it can be difficult to determine which mechanism causes the most damage.
To establish infection, a virus must enter a host cell. Once inside, it hijacks the cell’s machinery to replicate, eventually killing the cell and releasing more virus. This process not only damages host tissues, but also potently activates the immune system.
The immune system in turn unleashes powerful weapons to control the infection. However, if not carefully regulated, the immune response itself can cause collateral damage to host tissues and exacerbate disease severity.
More research on the host and viral factors that contribute to severe COVID-19 disease and death could provide important clues for clinicians and researchers in the search for new treatments.
Jay Bream, PhD, is an associate professor in Molecular Microbiology and Immunology at the Johns Hopkins Bloomberg School of Public Health.
-
Is it possible to be reinfected with the novel coronavirus?
Reinfection is always a possibility with a viral infection, particularly if you have a subclinical infection and don’t mount much of an immune response against it. Reinfection is also possible within the window after the first infection and before you develop antibodies. That window can vary from a couple of weeks to a few months, depending on how much your immune system was triggered.
We’ve now got a good population of people who have recovered from the virus. Serum samples from those patients can allow us to time exactly when they begin to develop antibodies and when they develop sufficient titers and neutralizing antibodies. This will help us determine what the window is for protection.
Before your immune system returns to normal, you can be infected by not just this virus, but by regular colds and flu. A couple of months may be a reasonable window of recovery, based on what we know right now.
Rachel Graham, PhD, is an assistant professor in the Department of Epidemiology in the UNC Gillings School of Global Public Health. She began actively studying coronaviruses just prior to the SARS-CoV pandemic in 2002–2003.
-
What is viral load, and does it mean doctors and nurses face greater risk of infection or getting more severely ill?
Viral load refers to the amount of virus detected in a sample, such as blood if the virus is present in blood, or the lungs if they can be sampled, and most commonly in nasal swabs taken for diagnosis. It is a quantitative measure of how much virus there is in a particular body fluid or site.
Certainly the higher the viral load the greater the risk of transmission to an uninfected person. But transmission is a complex process and the amount of virus a person is exposed to is only one variable.
While viral load can affect the risk of becoming infected, it is not typically associated with a more severe outcome of infection. That is determined by how well the virus replicates in the infected person, their general state of health, and perhaps genetic factors and unknown factors that change risk.
Raphael P. Viscidi, MD, is a virologist and professor of pediatrics and oncology at the Johns Hopkins University School of Medicine and is on faculty at the Johns Hopkins Bloomberg School of Public Health.
-
Is it safe to donate blood during the outbreak? Could someone get COVID-19 from a blood transfusion?
COVID-19 doesn’t pose any known risk to blood donors during the donation process or from attending blood drives.
Blood donation is a highly regulated, safe process—and most centers have implemented additional precautions including increased sanitation of donor areas, use of PPE, and social distancing to enhance their already-healthy environments. Additionally, since donors must be healthy on donation day, risk of exposure to sick individuals is extremely low.
While donors may worry that they could be infected but asymptomatic, respiratory viruses are not generally thought to be transmitted by blood transfusion. There are no reported cases to date of transfusion transmission of COVID-19.
Even during a shelter-in-place, people still require critical medical care. They will continue to be in car crashes, need emergency organ transplants and chemotherapy, and give birth to babies in critical condition. The need for blood is constant, and we continue to rely on blood donors’ generosity.
Harpreet Sandhu, MSHS, MBA, is the CEO and executive director of Stanford Blood Center and a board-certified clinical laboratory scientist with specialties in Transfusion and Transplantation medicine.
-
What is cryptic transmission, and what is its significance in the COVID-19 outbreak?
Cryptic transmission is the term that is used when there is no direct contact between person 1 shedding the virus and person 2 contracting it.
It is an important indicator of community prevalence of a virus. There is essentially enough circulating virus in a community to transmit the same strain of the virus between individuals who are not directly linked.
In the case of the COVID-19 outbreak, this term came into the lexicon after University of Washington researchers sequenced the COVID-19 genome from Snohomish County, Washington, which showed a direct genetic link from the first 2 cases in Washington though they had no known contact. This indicated there was significant community spread, and likely evidence the virus had been circulating for weeks by that point. As I noted on Twitter, the key takeaway is this is going to be a critical path for viral transmission given the potential infectivity prior to the manifestation of symptoms—and what will ultimately make it so hard to control the spread of the virus.
Ingrid Katz, MD, MHS, is Harvard Global Health Institute's associate faculty director, an assistant professor at Harvard Medical School, an associate physician at Brigham and Women’s Hospital, a research scientist at the Center for Global Health at Massachusetts General Hospital, and associate faculty at Ariadne Labs.
-
Given that coronaviruses can cause the common cold, does that mean humans likely have some protection against this new virus? Or are we immunologically "naive"?
Although it’s possible we could have pre-existing immunity if we were previously infected with “common cold” coronaviruses, there is no evidence that this is protective in people exposed to SARS-CoV-2 (the virus that causes COVID-19).
Unless I see data otherwise, I’d assume that most of us are immunologically “naive.” However, although we don’t know if it’s relevant to COVID-19 epidemiology, it has been shown that antibodies against SARS-CoV can block infection of cells with SARS-CoV-2 in vitro, so there is the possibility of protective cross-reactive immunity from closely related coronaviruses.
Angela Rasmussen, PhD is a virologist on the faculty at the Center for Infection and Immunity at the Columbia Mailman School of Public Health. She specializes in using systems biology approaches to study how a host responds to a virus infection and how this response contributes to disease severity and clinical outcome.
-
How do you go about creating a vaccine against a new virus?
Every virus has its unique challenges. In the case of n-coronavirus, the vaccine challenges are 2-fold. First, you have to interfere with the virus’s ability to dock with a specific receptor in the lungs called ACE2.
Then, you need to reduce the problem of antibody-dependent enhancement. ADE means that some respiratory virus vaccines can actually make things worse. There are multiple ways to solve this problem. One option is creating a vaccine that only uses parts of the pathogen to stimulate the immune system. One approach is to do this by producing recombinant protein subunit vaccines.
We have found that these vaccines that use a part of a protein of the virus (the spike protein) and known as the receptor binding domain (RBD) are optimal for 2 reasons: Recombinant proteins are a standard technology that has resulted in other licensed vaccines, including the hepatitis B and HPV vaccines; and it’s possible to produce this vaccine in abundance and at low cost.
Moreover, this approach, unlike many others, reduces ADE and has potential for being safe.
Peter Hotez, MD, PhD, is dean of the National School of Tropical Medicine at Baylor College of Medicine and Co-Director, Texas Children’s Hospital Center for Vaccine Development.
-
How does this particular coronavirus compare with other coronaviruses like SARS and MERS?
“We are learning more about the virus every day. On the continuum of the common cold to SARS, it’s now clear that the novel coronavirus is more contagious than SARS, but less deadly. We don’t yet know how much more contagious, or how much less deadly. The number of confirmed infections with nCoV has already far outpaced the total number of suspected SARS cases.”
Tom Frieden is President & CEO of Resolve to Save Lives, an initiative of Vital Strategies, and the former Director of the US CDC and Commissioner of the New York City Health Department.
Outbreak
-
Is the global disease surveillance system too dependent on the self-reporting of countries affected early on in an outbreak? How could it be strengthened?
The global community depends on countries being transparent about disease within their borders—but in practice countries have few incentives and deep disincentives to share this information. The 2005 International Health Regulations established the expectation that countries develop capacities to conduct surveillance to detect and rapidly report infectious disease events that could spread internationally—but enforcement is limited. We must acknowledge shortcomings in international agreements that hamper reporting, along with a shortage of funding to help countries build and maintain surveillance capacities.
Reactive trade and travel restrictions enacted following outbreak reports can create a chilling effect on reporting, too. Instead of pursuing these punitive actions, the international community should offer countries experiencing outbreaks aid to help contain the spread of disease at the source. We should also expand use of other data sources, such as media and unofficial reports, to help validate or expose problems in countries’ official disease reporting.
Jennifer B. Nuzzo, DrPH, SM, is an epidemiologist with the Johns Hopkins Bloomberg School of Public Health’s Center for Health Security.
-
What are 'excess deaths' and what do they tell us?
We are all going to die someday, so it is hard to know if a disease is just killing people who would have died soon anyway, or if it is actually increasing mortality. This is particularly true for a disease like COVID-19, which mostly kills older people.
Another issue that complicates our understanding of mortality in a population: Deaths—from coronavirus or other causes—are often unreported or attributed to the wrong cause.
“Excess deaths” are a way to try to get at the real burden of a widespread disease like COVID-19. There
are sophisticated ways to do this, but the basic idea is to compare death rates during the epidemic to seasonal averages. So, if 1,000 people usually die in March in my town, and 1,500 die this year, that is 500 excess deaths; and with no other explanation we would presume the excess is due to COVID-19.Justin Lessler is an associate professor of Epidemiology at the Johns Hopkins Bloomberg School of Public Health
-
How can researchers tell the difference between naturally occurring and lab-produced pathogens?
Hundreds of different coronaviruses have been identified, and their genomes have been at least partially sequenced. With coronaviruses, those facts help determine virus evolution.
Mutations occur randomly in any virus, but mutations that give the virus an advantage over other viruses eventually dominate a virus population. When you have hundreds of sequences of viruses from different animal species, you can actually line up the sequences and see how viruses relate to one another. You can make a “tree” showing those relationships—which viruses evolved from others—and how they have evolved naturally. All that points to a gradual evolution of viruses driven by random mutations and natural selection.
If, however, you uncover a sequence that is only associated with a different virus family—influenza, for example—in a coronavirus, and no other coronaviruses had a similar or related sequence, that would be evidence for some type of engineered virus.
Andrew Pekosz, PhD, is co-director of the Johns Hopkins Center of Excellence for Influenza Research and Surveillance and a professor of Molecular Microbiology and Immunology at the Johns Hopkins Bloomberg School of Public Health.
-
Can SARS-CoV-2 be controlled, eliminated, or eradicated?
In public health, 3 key terms describe disease prevention:
- Control is the reduction of transmission, illness or severe outcomes of a disease. Well-controlled diseases include tetanus and diphtheria.
- Elimination means a disease is completely controlled and no longer occurring naturally in a given geographic area. Polio, for example, has been eliminated in the Americas.
- Eradication is the complete global elimination of an infectious agent (such as a virus), such that it no longer exists in nature. Only one human pathogen—smallpox—has been eradicated.
Maintaining disease control and elimination usually requires ongoing public health intervention(s), such as vaccination, but once a disease has been eradicated, interventions are not needed.
In the case of COVID-19, vaccines will hopefully lead to control, but it is too soon to know if it could be eliminated.
One of the most important biological properties that dictates whether a pathogen can be eradicated is that it must only infect humans. SARS-CoV-2, the virus that causes COVID-19, can also infect animals; therefore, eradication of the pathogen will not be possible.
Jessica Atwell, PhD, is an assistant scientist in the Department of International Health of the Johns Hopkins Bloomberg School of Public Health.
-
With a given number of confirmed Covid-19 cases in a community, is there a way to estimate the number of actual cases?
Not reliably because the number of tests affects the number of confirmed cases: If you do more tests, you’ll find more cases.
A better—but still flawed—approach would be to use the number of COVID-19 deaths and back-calculate the number of infected cases. So, if there are 500 COVID deaths in a community and you assume a mortality rate of 1%, then that would indicate that there would be at least 50,000 cases. Why? Because 500 is 1% of 50,000. But this has problems, too. It doesn’t include recent infections; the number of COVID deaths may be under-reported; and it depends on the death rate. These points suggest 50,000 cases is likely an underestimate.
So, what do we do? We need good public health surveillance. We need to take representative samples of the community and test them. That’s the best way to get reliable estimates.Ron Brookmeyer, PhD, MS, is dean of the UCLA Fielding School of Public Health.
-
There have been news reports that the coronavirus epidemic will last for 18 months or longer and come in multiple waves. If so, how long will social distancing be necessary in that situation?
This pandemic will last until most people are immune, whether through vaccination or from having gotten the illness [COVID-19] and recovered. The 18-month figure comes from reports that we won’t have a vaccine in less than 18 months, but that would be in unprecedented, in record-breaking time. We’ll eventually have a vaccine, but that may be in 18 months or 5 years from now.
I think there will be waves of the epidemic across the US. What’s happening now in Seattle and New York, and to a lesser extent in San Francisco, will happen in Baltimore and Dallas at different times. Each wave will last a couple of months—from valley to peak to valley. As we begin to relax social distancing efforts—which we will have to do because society can’t stay like this—the disease will start to come back. The hope is that it will return more slowly because there are fewer susceptible hosts, we’ll have more ubiquitous testing, and more [targeted] interventions instead of the sledgehammer we’re using now.
Eric Toner, MD, is a senior scholar at the Johns Hopkins Center for Health Security at Johns Hopkins Bloomberg School of Public Health, with expertise in health care preparedness for catastrophic events, pandemic influenza, and medical response to bioterrorism. -
What’s the worst-case scenario for this pandemic?
There is already evidence of widening transmission of SARS-CoV-2 across the Southern Hemisphere, though the virus is currently taking its primary toll in the North. It is likely that 60-65% of Northern Hemisphere populations will be infected with the virus by July or August.
As the epidemics seem to diminish later in the summer, action will shift to the South, with COVID-19 sweeping across Latin America, Africa and the South Pacific, similarly infecting upwards of 60% of populations. And then by December, it will make a slow return to the Northern Hemisphere, creating a North/South cycle that will persist for years.
Adding additional fuel to the South’s fire will be high HIV infection rates, with more than a third of HIV-infected Africans, in particular, unaware of their status and therefore not on suppressive medication, and immunocompromised.
Laurie Garrett is a former senior fellow for global health at the Council on Foreign Relations and a Pulitzer Prize winning science writer.
-
How much will mortality rates vary from country-to-country given differing levels of health system preparedness and response resources?
Mortality rates will vary by country according to several factors. First, it will depend on the age structure of the population; Italy has the second oldest population in the world, which may partly explain the high mortality observed.
Health care availability (in terms of the number of hospital and intensive care beds) and accessibility (free versus paid) will also influence mortality. For example, low death rates in Germany and South Korea are partially attributed to the relatively high number of hospital beds per capita. Moreover, disparities in death rates between Hubei province—the location of Wuhan, where the outbreak first emerged—and other parts of China are thought to be due to the rapid case rise and resulting strain on health care resources in Hubei.
Lastly, a country’s testing policy will be an important determining factor. If there is widespread testing of community as well as hospital-based cases, mortality will be lower than if testing was solely focused on hospital cases.
Antonia Ho, MBChB, PhD, MRes, MSc, is an infectious disease physician and clinical senior lecturer and consultant in infectious diseases with the Institute of Infection, Immunity, and Inflammation at the MRC-Centre for Virus Research at the University of Glasgow.
-
When does an outbreak become a pandemic?
The word pandemic literally means “all people” in Greek. But clearly not all people become sick even in the worst pandemics. Epidemiologists typically mean an infectious disease epidemic that has spread or is spreading globally.
Usually we refer to a pandemic only when it involves a new disease. So, for example, we talk about an influenza pandemic when there is a new strain of flu spreading around the world. In contrast, we do not refer to the global outbreak of seasonal influenza as a pandemic because the strains are not new.
There is no strict definition of when an epidemic becomes a pandemic—but usually it means that the disease is actively spreading on several continents with likely continued spread to other continents.
Eric S. Toner, MD is a senior scholar with the Johns Hopkins Center for Health Security and a senior scientist in the Johns Hopkins Bloomberg School of Public Health, Department of Environmental Health and Engineering. He is an internist and emergency physician.
-
Why are wild animals believed to be the source of this outbreak?
About 60% of newly emerged and re-emerging pathogens share a common origin: the bodies of animals. Genetic and epidemiological evidence suggest that the novel coronavirus, like SARS, may have emerged from a so-called “wet market,” where wild species that would rarely encounter each other in nature are crammed together, allowing microbes to spread between species and into humans. China claimed to have cracked down on these markets after the SARS outbreak, but when I visited a few years later, it wasn’t hard to find one.
But such markets are only part of the problem. The loss of wildlife habitat around the world more generally is forcing wild species to cram into closer proximity to human settlements. Bats, for example, have been fingered as the source of Ebola, SARS, and a host of other pathogens. When we cut down the forests where they live, they come roost in our backyards and farms instead. It’s this kind of novel, intimate contact that provides opportunities for the microbes that live in their bodies to spread into ours.
Sonia Shah is a science journalist and author of Pandemic: tracking contagions from cholera to Ebola and beyond. Her new book, The Next Great Migration: the Beauty and Terror of Life on the Move, will be published in June 2020.
-
How do disease detectives find the source of an outbreak like this?
Once two or more people are identified, disease detectives (such as those in the CDC’s Epidemic Intelligence Service) look for what these people have in common. Do they live together? Work together? Shop at the same market? Points of overlap could indicate sources of the pathogen.
At the same time, infectious disease doctors and scientists try figure out what the pathogen is. In the case of the novel coronavirus, scientists isolated and genetically sequenced the virus, revealing its close relationship to SARS, which originated in bats but was transmitted to humans through another species.
Pinpointing the precise animal species will take time and a lot of testing: It took more than a year to identify civets as the intermediary host between bats and humans for SARS.
Michael Mina, MD, PhD, is an assistant professor in the Center for Communicable Disease Dynamics at Harvard T.H. Chan School of Public Health and associate medical director of Clinical Microbiology at Brigham and Women’s Hospital and Harvard Medical School.
-
What are super spreaders and how can they affect the trajectory of an outbreak?
Rather than using the term super spreaders (a person who infects a large number of people), we should think of them as super spreading events. Maybe a person is at the right time of infection and at the mall. Typhoid Mary infected many people because she was a cook.
Part of the reason we stopped SARS is that a lot of super spreading was happening in health care settings and when people really got their act together in terms of infection control and biocontainment, it nipped the epidemic in the bud.
Super spreading events have the largest influence an outbreak’s trajectory early on. If there’s only a few cases and one person then infects 10 others, it can make it start strong. Once an epidemic gets going and has 100 to 200 cases or more, the “law of large numbers” takes over—and it stops mattering so much.
Justin Lessler is an associate professor of Epidemiology at the Johns Hopkins Bloomberg School of Public Health.
-
What’s a reproductive number and what does it tell us about an outbreak’s future?
The reproductive number represents the average number of people that one infected person will infect. The reproductive number for a disease can change based on how infectious the pathogen is, the host population, and environmental factors.
To control an outbreak, the goal is to reduce a disease’s reproductive number to less than 1. If the reproductive number remains 1 or higher, the outbreak will continue. In the case of COVID-19, the estimated reproductive number is around 2.6, meaning the outbreak is expected to continue.
The reproductive number can be reduced by altering transmission dynamics—with social distancing, home isolation, quarantine, and use of personal protective equipment in health care settings. Over time as people are infected and recover—or if a vaccine becomes available (which may take months or years)—immunity in the population also reduces the effective reproductive number of a disease.
Michael T. Osterholm, PhD, MPH, is the director of the Center for Infectious Disease Research and Policy (CIDRAP), and a professor for the University of Minnesota’s School of Public Health, College of Science and Engineering, and Medical School. He is also the author of the 2017 book, Deadliest Enemy: Our War Against Killer Germs, and a member of the National Academy of Medicine and the Council of Foreign Relations.
-
What does successful risk communications look like?
When you think of containing an epidemic, from Ebola to coronavirus, labs and disease surveillance are often top of mind. Risk communications, however, is a key aspect in shaping the course of an epidemic, and how prepared people are to combat it.
People need timely, accurate and easy-to-understand information that encourages protective behavior without inciting panic. Information based on the changing risk of transmission and not politics, fear or stigma is critical.
As coronavirus spreads, government, media and others need to elevate accurate information sources and built community trust while combatting misinformation.
Amanda McClelland is the senior vice president, Prevent Epidemics at Resolve to Save Lives, an Initiative of Vital Strategies, and has more than 15 years of experience in international public health management and emergency response.
-
Could export goods transmit SARS-CoV-2 infection around the world?
The likelihood of getting infected with SARS-CoV-2 (the virus that causes COVID-19) through export goods originating from China or elsewhere is quite low. Although SARS-CoV-2 can survive on surfaces from 2 hours to 9 days, it is vulnerable to heat, changes in pH, and common disinfectants. Since SARS-CoV-2 is an enveloped virus (meaning it has a fragile outer layer), it is less stable and more susceptible to disinfectants. Therefore, the risk of an infected person contaminating commercial goods is low—and so is the risk of catching the disease from a package that has been transported and exposed to different conditions (and temperatures).
So, feel free to order that dress from China or those leather shoes from Italy. While you are at it, wash your hands and maybe wipe the surface with a disinfectant because informed preventive measures are what we need to stop both COVID-19 and the fear epidemic from spreading.
Sulzhan Bali, PhD, MS, is a public health specialist with an international financing institution. She has over a decade of work and research experience in health security, global response to epidemics, and infectious diseases. The views expressed here are personal.
-
What are some of the major challenges to global cooperation in this coronavirus outbreak?
Data transparency and political sensitivity are two of the most critical challenges to effective global cooperation on the COVID-19 outbreak—and they are deeply entwined.
China has a history of concealing, delaying or refusing to share data and information (this happened with SARS in 2002-2003 and in 2018, when China reportedly refused to share samples of a bird flu with pandemic potential). Leading global health agencies have praised China’s response to COVID-19, while other experts doubt the accuracy of the reported data. Data transparency is key to building much-needed trust—and preventing the misallocation of resources, which could slow the response.
Some countries in Asia—where China holds significant economic and political influence—have carefully crafted their public coronavirus responses, aware that criticizing China could hinder cooperation. And all stakeholders face a difficult task: balancing effective disease response with the political sensitivity necessary for a successful, cooperative, global response.
Sarah McCool, PhD, MPH, MHA is a clinical assistant professor of Health Policy & Behavioral Sciences at the Georgia State University School of Public Health in Atlanta, GA.
Response
-
What is antigen testing, what are the pros and cons, and why isn’t it being used more broadly?
Antigen tests detect current SARS-CoV-2 infections by identifying small pieces of telltale proteins, with results possible in as little as 15 minutes—much quicker than most tests.
Every test has strengths and weaknesses:- Polymerase chain reaction tests are very accurate but slow to process and require skilled lab workers.
- Antibody tests only pick up previous infections.
- Antigen tests are quick, inexpensive, and efficient—but while very specific for the virus (good at detecting infections and unlikely to produce false positives), they are less sensitive than PCR tests. Therefore, a negative antigen test should be followed up with a more sensitive test, such as PCR, to confirm the results—particularly when the pretest probability is high, per CDC guidelines.
Citing insufficient data, the WHO does not currently recommend antigen tests for clinical diagnosis, and they haven’t been widely used in the US. Some countries, such as India, offer them but require a PCR test to follow up negative results.Seema Yasmin, MD is director of the Stanford Health Communication Initiative and a clinical assistant professor at the Stanford University Department of Medicine. She is also a journalist and author.
-
Should students and young people volunteer on the COVID-19 medical frontline?
The COVID-19 response of many countries would fall apart without the participation of health care students and young people—one of the most prominent groups of COVID-19 responders on the frontline.
Involvement in the crisis response can be a very valuable learning experience for young people and early-career professionals while helping their communities. However, they can be taken advantage of—expected to take on heavy risks and responsibilities without adequate compensation or protection.
Institutions in charge must ensure decent and safe working conditions and proper personal protective equipment. And, in the case of non-voluntary work, young people must be paid fair salaries to prevent the exploitation of cheap youth labor.
Working under considerable stress and pressure often results in a significant impact on their physical and mental health. Appropriate prevention and support structures must be available and accessible for young people to be able to cope with these adverse effects.
Marián Sedlák, MUDr, is a resident in emergency medicine and a PhD student at the Pavol Jozef Šafárik University in Košice, Slovakia.
-
How can disaggregated data improve pandemic response, and what should be done to get more countries on board?
Disaggregating COVID-19 data by age, sex, gender, race, employment, migration status, housing conditions, and other relevant social stratifiers clarifies the complexities of the pandemic. It enables countries to adapt their response for different populations with varying degrees of vulnerability to improve health outcomes.
The first step is recognizing that populations in a country, city, and even neighborhood are not homogeneously affected. The next step involves examining the factors that differentiate these health outcomes through an intersectional analysis framework. A preliminary method is to further disaggregate data by multiple social stratifiers to get a clear picture of who is most vulnerable.
Politicians should be made aware of the inequitable pandemic outcomes, implement more effective evidence-informed policies, and give the decision-making power to public health experts—including diverse advisers who are aware of populations’ vulnerabilities. Lastly, they should adopt an explicit intersectional framework in their evaluation and adaptation of the pandemic response.
Zahra Zeinali, MD MPH, is a researcher at Global Health 50/50 and a fellow at The Rockefeller Foundation-Boston University 3-D Commission on Health Determinants, Data and Decision-making. -
Will COVID-19 make the coming flu season worse?
Potentially, Yes. For a number of reasons.
We are already seeing a rise of COVID-19 cases over the past month that are straining health systems. Once flu season rolls around this will add additional strain to those systems.
We could also see a lot more flu/COVID-19 coinfection than we think because the tests commonly used for SARS-CoV-2 have a high false-negative rate, and their reliability can vary based on the type of sample taken: swab, sputum, or saliva.
That sample can determine whether the virus is detected or missed. Case studies have shown that some in some instances, only samples of lower respiratory sputum produced a positive result.
With flu/COVID-19 coinfection, it’s unknown whether one virus is making patients sicker than the other, if they’re competing with each other, or if they’re acting in conjunction to make patients even sicker.
The best way to minimize the chance of coinfection: get a flu shot and wear a face covering.
Kishana Taylor, PhD, MS, is a postdoctoral scholar in the Department of Microbiology and Molecular Genetics at the Díaz-Muñoz Lab at the University of California, Davis, which focuses on the evolution of virus coinfection.
-
What is intersectional analysis, and how could it mitigate health inequities in a pandemic?
Intersectional analysis rejects one-dimensional approaches to examining forms of oppression. Instead, it considers how characteristics such as gender, race, class, ability, and sexuality interconnect to form complex axes of discrimination and privilege. These identities impact an individual’s risk of ill health and access to appropriate treatment, and it is critical that global health policy is responsive to this.
The need to apply an intersectional lens is even more acute in a pandemic response. In such crises, social and economic inequalities exacerbate existing inequities in access to health, including those relating to housing, occupation, care responsibilities, and citizenship status. By collecting and analysing data on how COVID-19 affects groups of people differently, global health actors can take measures to prevent (often already marginalized) groups from being left further behind. This is an essential first step towards an accountable, inclusive system that accurately reflects the diverse needs of the populations it serves.
Mireille Evagora-Campbell, MA, is a researcher at Global Health 50/50 where she promotes gender equality and health equity.
-
How does contact tracing vary in different countries and cultures?
The fundamentals of contact tracing—investigating, finding, supporting, and isolating cases—do not vary by country, but the methods differ.
In many low- and middle-income countries, so-called “shoe-leather epidemiologists” conduct contact tracing, traveling door-to-door to ask direct questions (wearing out their shoes in the process).
In China and South Korea, smartphone surveillance has been key to contact tracing efforts. In the West, where individual rights and privacy are paramount, contact tracing is a harder sell. But it is a critical public health tool.
In the US, ethical contact tracing means carefully balancing individual rights with public health considerations. Interventions that may compromise individual freedoms—such as contact tracing or mandatory vaccines—must meet a 3-pronged legal standard demonstrating:
- Utmost respect for individuals’ independence
- Benefits to society that outweigh the “costs” of impinging on individual privacy
- All members of society benefit—not just an individual group
Tolbert G. Nyenswah, LLB, MPH, is a senior research associate in the Department of International Health at the Johns Hopkins Bloomberg School of Public Health. He was the incident commander for the response to the 2014–2016 Ebola outbreak in Liberia, and a contributor to the Bloomberg School’s free contact tracing course on Coursera. -
What does it take to be a great contact tracer?
On a technical level, you don’t need to be a public health expert to become a contact tracer—but you need great communication and interviewing skills.
Contact tracers must have the ability to talk to, read, and connect to people who have tested positive for COVID-19 with empathy. A lot of this work is being done by phone, presenting extra challenges. Contact tracers need to be good at getting people to open up, while being as thorough as possible to determine potential exposures.
Mistrust is another challenge, especially with certain populations such as homeless people, those with mental health issues, and undocumented people—who have shown an increased reluctance to access public services recently. Contact tracers must be able to put them at ease and reassure them their names will not be used.
In many cities, contact tracers who speak foreign languages are in high demand, too.
Joann Schulte, DO, is the deputy health authority and medical director of the Dallas County Department of Public Health. -
What is contact tracing, why is it important, and how is it done?
Contract tracing is a core public health function that public health agencies have done for years. Diagnostic tests can confirm whether a person is infected with an illness. Contact tracing involves finding out who the infected person had contacts with so that those individuals can be alerted that they are at a risk of developing the illness and at risk of potentially infecting others in the community.During contact tracing, the contacts of the infected person are generally called up, asked if they're feeling sick, and advised to self-quarantine for a period of time. During the quarantine period, the health of the contacts can be monitored and health care or other services could be provided to them if they do develop symptoms. Also, it is important to make sure that people who have been exposed to the illness are not circulating in the community and further spreading the disease.
Anita Cicero, JD, is deputy director of the Center for Health Security at the Johns Hopkins Bloomberg School of Public Health.
-
Do health care workers present a risk to the community by returning home after work?
Health care workers are always very aware of the risks they face at work while caring for patients. During the COVID-19 pandemic, there is increased vigilance in health care settings to prevent infection of patients and health care workers. Hospital infection control programs are charged with protecting our health care workforce and the patient populations we serve every single day. For protection against COVID infection, meticulous attention to hand hygiene, routine face masking and social distancing also apply in the health care setting. In addition, health care workers are trained in the proper use and disposal of personal protective equipment and potentially contaminated materials, instructed not to come to work when sick, and if sick, are prioritized for COVID-19 testing.
With the appropriate attention to infection prevention practices that every health care facility must practice, health care workers do not pose an increased risk to the community than the public at-large.
We are all paying close attention to practices to protect ourselves, our families, and our communities while caring for patients during this challenging time.
Marisa Holubar, MD, MS, is a clinical associate professor of Medicine - Infectious Diseases at the Stanford School of Medicine.
Yvonne (Bonnie) Maldonado, MD, is senior associate dean for Faculty Development and Diversity; and a professor of Pediatrics (infectious diseases) and of Health Research and Policy at the Stanford School of Medicine.
-
Why will it likely take longer to develop a vaccine than a drug for COVID-19?
The development of vaccines and drugs for COVID-19 share common goals: to ensure safety and efficacy. These are often assessed through a series of studies, sometimes beginning with animal experiments, progressing through human phase 1, 2 and 3 clinical trials with increasing numbers of participants. However, it often takes much longer to develop and rigorously assess a vaccine. First, vaccines are usually targeted to healthy people, in contrast to drugs administered to people with disease. Larger and longer studies are often needed to ensure the safety of vaccines. Second, the outcomes of interest often take much longer to be measured. Vaccine efficacy and immunogenicity can take many months to measure accurately, whereas whether or not a treated patient improves can take days. And some vaccines require multiple doses spread out over months whereas drug treatment regimens typically are days to weeks. Once developed, it can also take longer to manufacture and deploy vaccines.
William Moss, MD, is executive director of the International Vaccine Access Center and a professor of Epidemiology at the Johns Hopkins Bloomberg School of Public Health.
-
Does the COVID-19 pandemic automatically mean setbacks for ongoing global health programs?
Consider the limitations or strain already on health systems in many of the countries where global health programs operate. Whether related to health services, surveillance, or supply chains, meeting public demand can be an ongoing challenge at baseline. To add an outbreak response in those settings could spur an outright collapse of essential resources. And that could have a ripple effect for people in need of care across a range of issues, not only those exposed to a novel disease.
Consider a woman who can no longer visit a local clinic to protect her from pregnancy complications. Or the person living with HIV, TB, or some other chronic condition who can no longer receive lifesaving medications, either because of a breakdown or diversion of the pipeline intended to provide those. Furthermore, these very populations are at greater risk of poor outcomes from a disease like COVID-19, creating a potentially vicious cycle.
That is why it's essential that policymakers and practitioners shore up resources that protect progress in other critical areas of global health, while preventing fallout from a new public health enemy. If we are vigilant, we can soften the blow.
Loyce Pace, MPH, is president and executive director of the Global Health Council.
-
What’s the most important thing that WHO can do in the fight against COVID-19?
WHO has reiterated to all countries that with early and aggressive measures, they can stop transmission and save lives. WHO must be the first entry point for reliable information on the virus and its spread. It also has the unique mandate to provide evidence-based guidance to help countries and individuals to assess and manage their risk and make decisions. This is even more critical now as countries should be preparing for sustained community transmission. WHO must also be able to support the most vulnerable countries. The world requires a comprehensive and coordinated approach as outlined in the Strategic Preparedness and Response Plan that WHO has issued: Establishing international coordination and operational support; scaling up country readiness and response operations; and accelerating priority research and innovation.That turns the question on its head: One of the most important things countries and financial organizations must now do is support WHO in order to protect us all.
Ilona Kickbusch, PhD, chair, Global Health Centre, Graduate Institute of International and Development Studies, Geneva, and member of the Global Preparedness Monitoring Board.
-
How can public health advocates encourage citizens to trust their advice in countries roiled by attacks on science?
Today’s communication environment is a sea of rapidly changing “information,” confusion and distrust. Events shift rapidly, and conflicting perspectives, opinions and statements and accusations of “fake news” are common. Science-based information, when inconvenient, can be contested as just another perspective while repetition is used to establish “facts.” In this environment, presenting public health information so it is trusted, understood and acted upon is difficult but possible.
- Trust is built over time. Establish credibility by being a reliable source over time so when a crisis occurs, people will turn to you.
- Focus on what people want to know; not just on what you want to communicate. One person’s important facts can be irrelevant to others.
- Make information accessible. Provide the points and their basis and context clearly.
- Work with others. Similar information stemming from multiple sources strengthens believability and credibility.
Keiji Fukuda, MD, MPH, is a clinical professor and director of the School of Public Health of The University of Hong Kong. Previously, he worked for the US CDC and the WHO.
-
What does “preparedness” in a country really mean?
Preparedness starts with funding. That’s how everything else gets done—by having resources available to prepare for these kinds of rare but highly impactful events.
Public health departments would use that money to ensure expertise in emergency and pandemic planning. That’s key not only for the public health preparedness, but for preparedness in hospitals and long-term care facilities as well.
The money could also be used for supplies. In the US, we’ve heard a lot of about the Strategic National Stockpile which contains critical medicines and supplies needed during public health disasters. Having the resources to ensure we have extra supplies on hand is crucial.
Preparedness also means having policies and guidance ready to pull off the shelf during crises, rather than starting from scratch. That could include telework policies at an institutional level, or advance thinking on actions like the triggers that would indicate a need to close or reopen schools.
Caitlin M. Rivers, PhD, MPH is a senior scholar with the Johns Hopkins Center for Health Security and an assistant professor in the Environmental Health and Engineering department of the Johns Hopkins Bloomberg School of Public Health.
-
In the absence of approved treatments, what can health care providers do?
Even without approved treatments, there are several key ways health care providers can care for people with COVID-19 and keep them alive:
- Control their symptoms: Give them medications that make having COVID-19 more tolerable—ones that control fever, cough, and other commonly associated symptoms.
- Provide intensive support to the body of a sick person as their immune system battles the infection: We see that some patients may become critically ill with this disease, hence they may need mechanical ventilation or urgent dialysis. There may be a role for technologies such as extracorporeal membrane oxygenation to help their lungs recover from acute respiratory distress syndrome.
- Treat other infections that COVID-19 patients may get, such as concurrent bacterial pneumonia because their lungs are not functioning as well as they can. In this case, clinicians will use antibiotics to help them recover.
Nahid Bhadelia, MD, MALD, is the medical director of the Special Pathogens Unit at Boston Medical Center and an associate professor in the Section of Infectious Diseases, National Emerging Infectious Diseases Laboratories, at Boston University School of Medicine. -
What is the best way to counter misinformation in the media?
The best way to counter misinformation in the media is with an aggressive onslaught of facts. During an outbreak, information may be shifting, guidance changing, and questions multiplying, but the process is guided by adherence to reality and logic. Uncertainty is not an excuse for entertaining arbitrary assertions offered in defiance of the need for evidence. They should be identified as such and dismissed.
Experts, in addition to relating facts, should also explain the evidence that supports their conclusions and how recommendations are rooted in that evidence. This is a daunting task, as it involves more than information dissemination. It requires attention to what counts as evidence and an understanding of how to evaluate competing claims—some of which are grounded in evidence and some of which clearly are not.
Amesh Adalja, MD, is a senior scholar at the Johns Hopkins Center for Health Security.
-
What is it like inside a hospital biocontainment room?
At first glance, patient rooms in the Johns Hopkins Biocontainment Unit look no different than any hospital patient room—until you see the doors. They’re color-coded for health care worker safety. The colors signify required safety procedures to gain entry to a room. Red, for example, might alert a provider to change their personal protective gear.
We work so hard to make sure we can safely care for any patient, at any time, and simple safety cues like our doors help us do just that.
The design of the 7,900 square-foot unit, including three patient rooms, an onsite lab, shower facilities and clean-in/clean-out anterooms, helps us care for patients safely while protecting our staff and our community. A patient might be feeling scared and disoriented, so making sure they are safe and cared for is the number one priority of our team.
Lauren Sauer, MSc, is the director of Research with the Johns Hopkins Biocontainment Unit and director of Operations with Johns Hopkins Office of Critical Event Preparedness and Response.
-
What’s the best way to respond to the coronavirus outbreak?
Early in a coronavirus outbreak, unknowns are a given. But the global health community can’t afford to wait to see if a best- or worst-case scenario unfolds. Some post-haste priorities:
- Vaccine development: Make this is a top priority. Vaccines can dramatically slow disease spread though they can take at least a year to develop. Plans for large-scale production at different sites worldwide are also needed.
- Find treatments: Test possible antivirals—such as flu and HIV medications—for treatment options.
- Expand diagnostic capacity: Manufacture and distribute rapid diagnostic kits so cases can be identified quickly.
- Boost hospital readiness: Strengthen infection control procedures, train health workers, and keep masks, gowns, and gloves stocked.
- Communicate: Share facts (and unknowns) clearly with the public, and resist the temptation to withhold bad news.
If the virus is ultimately less lethal than feared, or more easily contained, the extra effort will pay off when the next one strikes.
Tom Inglesby, MD is the director of the Center for Health Security of the Johns Hopkins Bloomberg School of Public Health. This perspective was adapted from a piece he wrote in Foreign Affairs.
-
Can travel restrictions and quarantines stem the spread of the coronavirus?
Travel bans can’t keep all cases of the virus out of a country. As the epidemic expands, cases may originate in any number of countries. We may already have unrecognized cases in the US.
Travel bans can actually make us less safe. They can make countries facing restrictions not want to share information about their outbreaks. They can disrupt the distribution of supplies needed to control the epidemic. Similarly, as we saw with the US’s Ebola response in 2014, quarantining returning travelers makes doctors and nurses less likely to volunteer to serve in affected countries.
This virus is likely past the point of containment. We need to focus on mitigating its impact by speeding the development of diagnostic tools, vaccines, and drugs to treat infections.
Jennifer B. Nuzzo, DrPH, SM, is an epidemiologist with the Johns Hopkins Bloomberg School of Public Health’s Center for Health Security.
-
What should a country like the US be doing to prepare when an outbreak like this begins to spread globally?
“Beginning preparedness activities when an epidemics hits is too late. Although the US has a relatively strong health system, we need to be better prepared for an epidemic, particularly by strengthening state and local health departments and connections with health care providers and facilities. But we can’t protect ourselves only within our own borders. Our biggest vulnerability is spread in countries with weak health systems – viruses don’t need visas. The US should double down on support for countries in Africa and Asia so the health workers in these countries can find, stop and prevent epidemics. In the US and globally, there are important and simple things we can do that will prevent illness now and also protect against coronavirus: improve hand hygiene (handwashing), cough hygiene (cover coughs), don’t expose others if we’re feeling ill, and improve health care infection control.”
Tom Frieden is president & CEO of Resolve to Save Lives, an initiative of Vital Strategies, and the former director of the US CDC and commissioner of the New York City Health Department.
-
Are strong national health systems all we need for pandemic preparedness?
Strong health systems are certainly a crucial foundation for preparedness. All countries, rich or poor, need to have a set of core national preparedness capabilities. For example, they need strong surveillance systems in place that can detect infectious diseases with pandemic potential, robust case detection, and effective contact tracing (i.e., identifying and reaching those who may have been in contact with an infected person).
But that’s only part of the story. By definition, pandemics cross national boundaries—they are global in nature and they require a global response, not just a national one. A whole set of “transnational” activities, called global public goods, is another critical plank in pandemic preparedness. These require collective funding by all countries. Such goods include developing medical countermeasures like pandemic vaccines, diagnostics, and treatments, stockpiling of medical supplies (including personal protective equipment), and ensuring that there is global “surge capacity” to rapidly scale up production and distribution of vaccines.
Gavin Yamey, MD, MPH, MA, is a professor of the practice of global health and public policy and director of Duke University’s Center for Policy Impact in Global Health.
-
What do frontline health care workers need most when they face an outbreak like this?
Health care workers are our first line of defense against disease, whether coronavirus or otherwise. In order to safely and effectively do their jobs they need to both have proper training and the right protective equipment. This keeps them safe from infection in “peace time” and during a large outbreak like we have now.
Health care workers are often the first affected by these types of outbreaks and to some extent can act as a canary in the coalmine for how infectious a new disease outbreak is. In the past, health care workers have died from infections and also amplified initial cases spreading the outbreak quickly. If we are to protect health workers and limit transmission, we must do more to ensure the right training and the right equipment are available all the time and not just once an outbreak has started.
Health workers are making heroic efforts in China, where they have converged on the epicenter. They can only protect us if they are protected.
Amanda McClelland is the senior vice president, Prevent Epidemics at Resolve to Save Lives, an Initiative of Vital Strategies, and has more than 15 years of experience in international public health management and emergency response.
-
What are the ethical considerations of using quarantines?
The tools of public health during suspected infectious outbreaks include limits or restrictions on the movement of individual citizens, ranging from travel bans, to closure of businesses and schools, to isolation of individuals in their homes, to forced quarantine in medical facilities.
The goal in implementing public health measures during suspected outbreaks is to balance the freedom of individuals against the restrictions on freedom required to achieve legitimate protections of the public's health, with public and transparent justification of policy decisions.
Whatever restrictions are implemented should be the least restrictive to accomplish the stated public health goals. Quarantine is considered a measure of last resort given the severe restrictions it imposes on individual liberty, and when misused or ineffective can severely undermine trust in government.
Jeffrey Kahn, PhD, MPH, is the Andreas C. Dracopoulos Director of the Johns Hopkins Berman Institute of Bioethics.
Minimize Your Risk
-
How young is too young for a child to wear a mask? And does not wearing a mask put infants and young children—and their families—at special risk?
The American Academy of Pediatrics recommendation is that cloth face coverings are safe and effective for children over the age of 2 years, including the vast majority of children with special health conditions. Face coverings are especially important when social distancing is hard to do. Children under 2 years old should not wear cloth face coverings because of suffocation risk.
Across the world, there has been a recent rise in reported COVID-19 cases in children confirming that they can be infected. Fortunately, children tend to have milder symptoms and rarely need to be hospitalized. It remains unclear whether young children infected with COVID-19 are more or less likely to spread it to others. Face coverings will be essential for children to safely return to school, childcare or other group settings.
Don't hesitate to talk with your child's physician if you have any questions about your child wearing cloth face coverings.
Theresa Guilbert, MD, MS, is a professor of Pediatrics at the University of Cincinnati and director of the Asthma Center in the Division of Pulmonology Medicine at Cincinnati Children's Hospital & Medical Center.
-
Do we need to worry about catching COVID-19 from toilets?
When toilets flush, the turbulent water aerosolizes fecal matter, creating particles known as bioaerosols. Bioaerosols can linger in the air until they are removed via bathroom exhaust or air filtration, settle on surfaces, or are inhaled.
Viable SARS-CoV-2 has been detected in stool samples, making bioaerosols from toilets a potential exposure pathway. However, there are no confirmed reports of transmission this way. Taking simple precautions—running bathroom ventilation or opening windows, closing the toilet lid before flushing, and washing hands—is prudent.
In 2003, sewage vapors were linked to an apartment building SARS outbreak in China. A recent case study related to SARS-CoV-2 reported similar findings. In both cases, empty trapways (called p- or u-traps) in floor drains failed to stop vapors from wafting throughout building pipes and into other apartments. Floor drains and other infrequently-used drains should be filled with a little water to prevent sewage vapor from passing.
Joseph Allen, DSc, MPH, is an associate professor and director of the Healthy Buildings program at Harvard T.H. Chan School of Public Health, and co-author of Healthy Buildings: How Indoor Spaces Drive Performance and Productivity. -
What are my rights as an employee if my job re-opens for in-person working, and I am not comfortable with their policy?
All employees have a legal right to a safe work environment.
If you’re uncomfortable with your employer’s COVID-19 safety protocols, there are ways to take action:
- Most employers aim to do the right thing—so first try resolving the issue internally. By law, you can’t be retaliated against for expressing these concerns.
- There’s safety in numbers—so join forces with colleagues.
- If you get fired for refusing to work in an unsafe environment, you should be entitled to unemployment compensation. Be prepared for a legal battle if your employer contests the claim.
- You can file a formal complaint with the Occupational Safety and Health Administration—but don’t expect a speedy resolution.
- Know your area: Absent robust federal action, some states are taking a more active role to protect workers.
- Look to labor unions: During the pandemic, some are stepping up to help workers even if they aren’t members.
—Sharon Block is executive director of the Labor and Worklife Program at Harvard Law School
-
Can Halloween trick-or-treating be safe this year?
Trick-or-treating, like any activity during the pandemic, cannot be made zero-risk—but it can be made relatively safe.
For example, trick-or-treaters can practice social distancing between groups, sanitize their hands between houses, and wear face coverings (which are likely part of many costumes in some form already).
Those passing out candy can also wear masks—or just leave dishes or individual bags of candy out (if they are worried about exposure at the door). Transmission of this virus does not occur with fleeting contact; letting children trick-or-treat is 1 type of activity where I think the risk of transmission is manageable.
Amesh Adalja, MD, is a senior scholar at the Johns Hopkins Center for Health Security. -
How can I assess whether measures to limit the spread of COVID-19 at my child’s school or college are sufficient?
To size up a school’s commitment to safety, look for a number of measures. Most importantly, is physical distancing emphasized? Will students be kept in small, fixed groups?
It’s really advisable to hold lessons outdoors if possible. Otherwise, ventilation is key—aiming to completely replace indoor air ~3 times/hour. 2 windows (or a window and a door) open should suffice. But keep in mind: In Jerusalem, such plans were abandoned when a heat wave hit.
Getting to class presents risks, too. Denmark eased hallway crowding with staggered entrance and exit times. And think about how children travel to school: It does little good to group kids carefully in classroom pods if they mix freely taking public transportation on their way in.
There should also be routine COVID-19 testing of teachers. Does the school have a plan for responding to a positive case, and how vulnerable students and teachers are treated?
Ronit Calderon-Margalit, MD, MPH, is a professor of Epidemiology and director of the International Master of Public Health program at Hadassah-Hebrew University Braun School of Public Health in Jerusalem. -
Should I get tested if I don’t have symptoms?
Your decision about whether to get tested will depend on personal factors: whether you have recently been around someone who is infected, rates of transmission in your area, whether you or someone you live with is high-risk, or whether you plan to visit someone not previously in your “bubble.”
It also depends on availability of testing in your area. If testing turnaround times are slow, the results may be moot by the time you get them.
Ideally, people without symptoms would have easy access to inexpensive rapid tests—similar to over-the-counter pregnancy tests.
These less-sensitive tests may miss lower levels of infection, but they’re pretty good at picking up infection when virus levels are at their highest, which is considered the most infectious period. This approach could help spot cases that would be missed by PCR testing—such as people who were discouraged from getting tested or couldn’t get an appointment.
–Natalie Dean is an assistant professor of Biostatistcs at the University of Florida specializing in emerging infectious diseases. -
How can I know which COVID-19 tests are safe and reliable, with so many on the market?
Safety isn’t a big concern for taking a COVID-19 test; it’s how the test results change behavior that might affect safety.
There are 2 categories of COVID-19 tests: diagnostic tests to see if you currently have the disease, and antibody tests to find out if you were infected previously. The most important are diagnostic tests, because if you have the disease you need to take steps to avoid spreading it to others.
Antibody tests are in high demand, because many people think that if they already had COVID-19, they won’t get it again, and they can stop physical distancing—but that’s unsafe because we don’t know yet if reinfection is possible. Antibody tests can also give false positive results, so people might think they had it and aren’t at risk of catching it again—and they’d be wrong. That’s why it’s best to wear a mask and take sensible precautions.
Gigi Kwik Gronvall, PhD, is an associate professor in the Environmental Health and Engineering program and a senior scholar at the Johns Hopkins Center for Health Security.
-
What’s the difference between face masks and face shields?
Face shields are transparent plastic devices that cover a person’s eyes, mouth, and nose, affixed to a headband. As such, they offer eye protection and prevent an individual from touching their face, unlike masks.
This likely leads to face shields being protective—both to the wearer, and to those around infected wearers. Studies with proper face shields that extend to the chin and wrap around the sides of the face have demonstrated good protection from infection in cough simulators. Face shields are also more comfortable to wear and easier to wear correctly, unlike many masks that people are prone to wear with their nose protruding.
While recommendations diverge, I, and some others, prefer face shields because of their eye protection and ease of wearing. Though we don’t yet have strong data, face shields are emerging as an alternative or supplement to face masks and are clearly better than an improperly worn face mask.
Amesh Adalja, MD, is a senior scholar at the Johns Hopkins Center for Health Security.
-
Are smokers at greater risk of catching or becoming seriously ill from COVID-19, and how can they minimize their risk?
It is well established that people who smoke are more vulnerable to infection, for example, 5 times as likely to get the flu and twice as likely to get pneumonia. We’re still at a relatively early stage in the pandemic, without complete data, but the best evidence does point to a link between smoking and COVID-19.
The UK Zoe symptom study, of 2.4 million+ people who recorded symptoms in an App, found that current smokers were more likely to report classic COVID-19 symptoms (cough, fever and breathlessness)—and also to report more symptoms, including anosmia (the loss of sense of smell) which appears to be very specific to COVID-19.
Apart from direct links, it is a good idea to #QuitForCOVID as this rapidly reduces an individual’s risk of other acute health problems like heart attacks and strokes. This is especially important at a time when health systems are under stress.
Nicholas Hopkinson, MD, is a Reader in Respiratory Medicine on the faculty of Imperial College, London.
-
Is the use of tear gas or pepper spray during the COVID-19 pandemic extra dangerous? How can people protect themselves?
Tear gas and pepper spray are very painful. Your eyes, skin, nose and mouth burn. Exposed people cry, cough and sometimes vomit. You experience shortness of breath and your lungs produce large amounts of mucus. If a person who is unaware of having an active COVID-19 infection is exposed, he or she may spread the virus more widely to others.
Tear gas may also make it easier for SARS-CoV-2 to infect people. US military scientists have found that recruits exposed to tear gas in training develop lung injury and are more prone to respiratory illnesses including viral influenza, as well as pneumonia and bronchitis, which viruses can cause. While not confirmed for COVID-19 directly, it is common knowledge that chemical lung exposures increase the infection risk.
Always wear a mask, especially during crowded protests. Protect your eyes with safety goggles or glasses in case you are hit by objects, or where there is dust and smoke. When the police use tear gas, move away quickly. If you are exposed, remove your clothes and shower with lots of water and soap. If your eyes are exposed, rinse 10-15 minutes with plenty of plain water.
Sven-Eric Jordt, PhD, is associate professor of Anesthesiology, Pharmacology & Cancer Biology at Duke University School of Medicine and faculty in Duke’s Integrated Toxicology and Environmental Health Program.
-
Are people who get early treatment more likely to recover faster or avoid severe illness, and how should that inform testing guidelines?
Earlier diagnosis can help in 2 ways:
We now know that certain therapies that have shown promise in treatment of COVID-19 work better when given earlier in the disease course, including remdesivir and convalescent plasma.
This is likely because damage from the disease occurs not only from the direct action of the virus, but also the impact of overactivation of the immune system in response to the infection, which leads to inflammation, and finally from abnormal blood clotting as a result of multiple factors. It makes sense that if we can catch patients as early as possible and keep their bodies from going down this path, it may result in better outcomes.
Diagnosing those with COVID-19 symptoms in the community as early as possible also allows public health officials to advise patients to isolate, to ensure that infected patients are not passing on the disease to others.
Nahid Bhadelia, MD, MALD, is the medical director of the Special Pathogens Unit at Boston Medical Center and an associate professor in the Section of Infectious Diseases, National Emerging Infectious Diseases Laboratories, at Boston University School of Medicine.
-
If I have a heart condition what precautions should I take to avoid serious COVID-19 illness?
It is very important to continue taking heart medications as prescribed and urgently address any cardiac symptoms that arise.
Early in the outbreak, there were concerns that Angiotensin-converting-enzyme inhibitors (ACE inhibitors) may increase the risk of COVID-19 illness, but medical organizations have concluded that they pose no increased risk—and have proven lifesaving benefits.
However, for patients who require a ventilator, it may be necessary to adjust or stop certain cardiac medications based on blood pressure and heart status.
Symptoms for COVID-19 and an active cardiac issue—such as shortness of breath and chest discomfort—can be similar. If heart medications are not being taken consistently to control cardiac symptoms, it is more difficult to distinguish between COVID-19 and a cardiac event.
While some patients are understandably apprehensive about seeking care during the pandemic, it is crucial to not delay. Research in Italy showed that visits to cardiac units halved during the outbreak—coinciding with an increase in out-of-hospital deaths from heart attacks.Shelley Hankins, MD, is an associate professor of Medicine at Penn State Medical Center at Hershey, specializing in advanced heart failure and heart transplantation.
-
Can COVID-19 spread through water in pools, hot tubs or water parks? When will it be safe to go to public swimming pools?
Water in pools, hot tubs, and water parks should be disinfected to reduce the risk of swimmer exposure to microbial pathogens. In pools that properly apply disinfectants, SARS-CoV-2 will probably be quickly inactivated—making the risk of COVID-19 spread from water likely to be quite low.
However, this does not affect the possibility of COVID-19 spread by airborne transmission or from contaminated surfaces. Therefore, social distancing and proper hygiene practices will be important to minimize transmission of COVID-19 in pools. This presents a significant social/behavioral problem, as swimming tends to be a highly social activity.
For pools to be safe to use (i.e., present an acceptably low risk of disease transmission) during this pandemic, they will need to adhere to conventional operational and maintenance standards—but with additional restrictions, such as requiring poolside patrons to wear masks, limiting attendance, and actively discouraging people from congregating in and around the pool.
Ernest R. Blatchley III, PhD, PE, BCEE, is the Lee A. Rieth Professor in Environmental Engineering at Purdue University. His research focuses on water treatment and water quality, including extensive research on these topics in swimming pools.
-
If I take immune-suppressing medication, should I stop so I'll have a better chance of avoiding COVID-19 infection?
Research into COVID-19 and patients who take immunosuppressing drugs is still scarce. However, investigations from Italy found that patients with systemic autoimmune diseases do not seem to have an increased risk of becoming infected.
Needless to say, immunosuppression impairs innate and adaptive immunity and is a risk factor for severe COVID-19 illness. While this holds true for the majority of patients, a subset of COVID-19 patients exhibit “hyper-inflammation"— an immune system activation triggered by the virus. The impact of initiating immunosuppression in these COVID-19 patients is being tested in several ongoing clinical trials.
Patients should consult with their physician on the need to take immune system-suppressing medication. Some circumstances require long-term intake of immunosuppressing drugs, [such as with] organ transplantation and abrupt withdrawal poses a risk to patients to have organ failure due to rejection. This in turn would lead to hospitalization and the need to intensify treatment—increasing not only the chance of becoming infected but also the risk of a severe COVID-19 disease course.
Andreas Kronbichler, MD, PhD, is a researcher at the Medical University Innsbruck, specializing in glomerular diseases and autoimmunity.
-
Why is diabetes considered a risk for severe COVID-19?
For people with diabetes, factors that potentially play a role in increasing their risk of developing a more serious case of COVID-19 include:
- The presence of chronic medical conditions such as cardiovascular disease, hypertension, and obesity that also increase the risk for COVID-19
- Impaired function of white blood cells that fight infection, and an exaggerated inflammatory response by the body toward the SARS-CoV-2 virus
- Increased expression of an enzyme (angiotensin-converting enzyme 2) in the lungs, heart, kidneys, and pancreas that acts as a portal for the novel coronavirus to enter human cells
To stay healthy, optimal diabetes management is important, including controlling blood pressure and cholesterol levels. People with diabetes should stay hydrated, carefully record blood glucose and ketone readings, and—if a person develops symptoms such as fever, cough, or shortness of breath—contact their health care provider immediately.
Ranganath Muniyappa, MD, PhD, is a senior research physician at the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. He published “COVID-19 pandemic, coronaviruses, and diabetes mellitus,” on March 31, 2020, in the American Journal of Physiology.
-
Can my kids go and play with friends?
It really is best to limit interactions as much as we can, and arranging play dates is generally not a good idea. Every time we get together with another person we’re not just exposed to each other—we’re also exposed to all of the other people that they have come into contact with.
If you really need the help, arrange play dates safely by asking your friends and family to keep their circle of contacts small. As a guideline, keep play dates between no more than 2 families.
I have a 1-year-old, and I’m trying to go for lots of walks with him. We go to the park, but we don’t play on the equipment any longer—instead I let him run around in the field as much as he wants. We keep our distance from other people, but we say hello from afar and kick a ball around instead.
Crystal Watson, PhD, MPH is a senior scholar at the Johns Hopkins Center for Health Security and an assistant professor in the Department of Environmental Health and Engineering at the Johns Hopkins Bloomberg School of Public Health.
-
As COVID-19 symptoms mimic those of common cold and flu viruses, how do you know when you should seek testing or special care?
The symptoms of COVID-19—including fever, cough, and difficulty breathing—are similar to those of other cold and flu viruses. At this moment, the decision to test for COVID-19 in the US depends on both the patient’s clinical status and what is happening in a particular geographic location. A history of travel, especially international travel to one of the most affected areas, is still important, but this is evolving as the outbreak develops domestically. Close contact with someone who traveled to those areas or with someone who has been diagnosed with COVID-19 are other considerations.
The evaluation of cold and flu symptoms will often include testing for routine respiratory viruses as well, especially influenza. In general, if you do not have symptoms and would not ordinarily seek medical care based on how you feel now, you do not need evaluation or testing for COVID-19.
Preeti N. Malani, MD, MSJ, is the chief health officer and a professor of Medicine in the Division of Infectious Diseases at the University of Michigan.
-
What should the average person in a non-outbreak area be doing to prepare?
The CDC believes it is likely that COVID-19 will cause a pandemic, but there are steps that the public can take to protect and prepare themselves.
First, it is important to stay informed and follow instructions issued by your local or state health department and the CDC. Basic infection control measures still apply in this scenario. Practicing good handwashing techniques or using hand sanitizer, avoiding people who are ill, and staying home when you are sick are all effective measures.
A pandemic could interrupt supply chains and result in closures at local businesses, meaning it may be prudent to stock reserves of critical supplies. Examples include extra prescription medications, asthma relief inhalers, over-the-counter anti-fever and pain medications, non-perishable food items, household cleaning supplies, and toiletries. However, do not hoard - this could create shortages.
Michael T. Osterholm, PhD, MPH, is the director of the Center for Infectious Disease Research and Policy (CIDRAP), and a professor for the University of Minnesota’s School of Public Health, College of Science and Engineering, and Medical School. He is also the author of the 2017 book, Deadliest Enemy: Our War Against Killer Germs, and a member of the National Academy of Medicine and the Council of Foreign Relations.
-
What precautions should I take when I have to go out to get food?
The majority of the transmission is happening through respiratory droplets that we may inhale from close contact with one another. To avoid crowds, be strategic about the time and the day of week that you go out to get food. Even now, shopping centers get busier on weekends. If the store is crowded, try again later.
As the CDC recommends, unless you’re treating a patient, use a homemade face cover when you go out in public. Medical masks must be saved for health workers who need them desperately. Also, use hand sanitizer or wash your hands as soon as possible after returning from the grocery store. If you decide to wear gloves, treat them like you would your bare hands. Immediately dispose of the gloves after an activity, and then wash your hands.
And, if you receive take-out at home, have it left at the door to help protect delivery people, who are doing a great service for us.
Crystal Watson, PhD, MPH is a senior scholar at the Johns Hopkins Center for Health Security and an assistant professor in the Department of Environmental Health and Engineering at the Johns Hopkins Bloomberg School of Public Health.
-
What are the special risks of COVID-19 to pregnant women?
Infection rate and progression to severe disease in pregnant women is similar to that in nonpregnant adult women. The same protective measures against transmission of the virus apply to both.
So far, no transmission from mother to fetus has been described. Vaginal delivery should be encouraged when both the mother and the baby are not severely sick. Strict protective measures (facemasks, hand hygiene) must be observed to protect the newborn and the personnel during and after childbirth.
Separation of the mother and baby and breastfeeding should be discussed on a case-by-case basis with the mother. The newborn should be protected from infection by the mother as much as possible. If the mother wishes to express her milk or breastfeed, disinfection of the breast should be added to the protection methods mentioned above.
We have launched an international registry for women exposed to COVID-19 and welcome any medical center and maternity to join. (If you are a patient interested in sharing your data, please suggest that your doctors contact Dr. Baud.)David Baud, MD, PhD, is head of obstetric service in the Department of Woman-Mother-Child at Lausanne University Hospital, where his research team studies emerging infections in the OB/GYN field.
-
Could export goods transmit SARS-CoV-2 infection around the world?
The likelihood of getting infected with SARS-CoV-2 (the virus that causes COVID-19) through export goods originating from China or elsewhere is quite low. Although SARS-CoV-2 can survive on surfaces from 2 hours to 9 days, it is vulnerable to heat, changes in pH, and common disinfectants. Since SARS-CoV-2 is an enveloped virus (meaning it has a fragile outer layer), it is less stable and more susceptible to disinfectants. Therefore, the risk of an infected person contaminating commercial goods is low—and so is the risk of catching the disease from a package that has been transported and exposed to different conditions (and temperatures).
So, feel free to order that dress from China or those leather shoes from Italy. While you are at it, wash your hands and maybe wipe the surface with a disinfectant because informed preventive measures are what we need to stop both COVID-19 and the fear epidemic from spreading.
Sulzhan Bali, PhD, MS, is a public health specialist with an international financing institution. She has over a decade of work and research experience in health security, global response to epidemics, and infectious diseases. The views expressed here are personal.
-
Can the new coronavirus be transmitted via paper money?
Cash can be contaminated with potential bacterial pathogens, but there is little information about viruses on cash in general—and nothing about contamination with SARS-CoV-2, the virus that causes COVID-19.
SARS-CoV-2 is spread by person-to-person contact—not normally by touching fomites (objects that may be contaminated with, and help transmit, infectious organisms) like cash. And, it’s unclear how long COVID-19 remains viable on surfaces—ranging from a few minutes to hours to potentially days depending on the temperature, humidity and surface type. Switching from cash to plastic has not been proven more protective, either, except perhaps by reducing person-to person hand exposure.
Some countries are washing or disinfecting cash, but there is no data demonstrating how this process works. The best practice is social distancing: limiting person-to-person contact by shutting down schools, bars, and other crowded places. That is what will slow infections, prevent health care systems from overloading, and reduce deaths. That is why everyone should do their part and embrace social distancing rather than worrying about using money or credit cards.
Marilyn Roberts, PhD, MS, is a microbioligist and professor of Environmental and Occupational Health Sciences, an adjunct professor of Global Health, and an adjunct professor of Pediatric Dentistry at the University of Washington School of Public Health.
This scanning electron microscope image shows SARS-CoV-2 (round magenta objects), also known as COVID-19, emerging from the surface of cells cultured in the lab. Image: NIAID-RML