Our Crowded EDs Speak Volumes About Our Broken Health System
As an emergency medicine physician, I find some of the toughest days in the emergency department are on holidays.
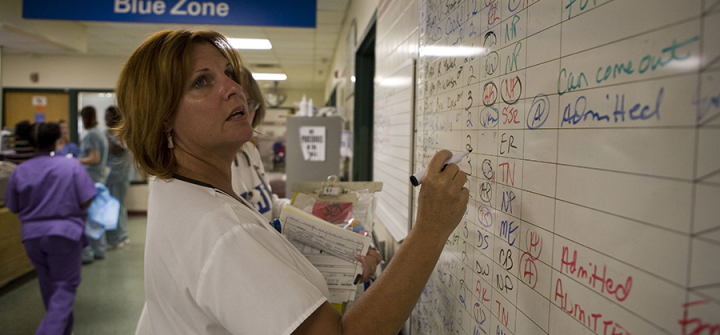
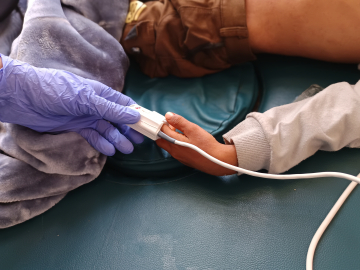
This year’s New Year’s Day was no exception. Waiting rooms were filled with adults and children who were sick or injured and didn’t know where else to go. A few were gravely ill or hurt; they took priority.
But many patients seeking emergency care aren’t in crisis. Some are referred from other clinics that don’t have the equipment or training to address their needs. Some are there because other clinics are closed or full, or because they have been waiting to get an appointment and just couldn’t wait any longer. Still others come because they can’t afford or access care anywhere else, or insurance has not approved tests that their physicians recommended unless they are emergencies.
Working these holiday shifts leaves me feeling incredibly frustrated. The fact that patients in our emergency department waiting rooms are there at all—spending hours waiting for help—is a troubling sign that our health care system is broken.
In the US, we are fortunate to have round-the-clock access to outstanding emergency care. Emergency doctors and nurses are trained to intervene in life-and-death situations. But what does it say about our health care system that this highly specialized and expensive form of care is also the most easily accessible?
So many of the patients we see in the emergency department could have been helped by primary or urgent care, had those options been more readily available to them. Many others could have avoided health problems entirely with more proactive preventive care. Yet these systems of care, specifically prevention-driven primary care—so essential for an efficient health care system—are often inaccessible to patients who need them, particularly those who are poor or don’t have adequate health insurance. In the US, even the recent explosion of urgent care clinics are more successful in creating profit than they are reducing ED burden. Urgent cares are not always geographically accessible to patients, require insurance and or large co-pays, and continue to focus on urgent solutions rather than a preventive focus.
And even when patients do have insurance, obtaining appointments with physicians and receiving health insurance approvals for “non-emergency diagnostics” limit their access to much needed care.
This is not an inevitable condition of a complex health care system. In my nonclinical work, I train emergency medicine physicians and study health systems in many parts of the world—including Brazil, Tanzania, and Eswatini. Through this work, I’ve seen firsthand how other countries are figuring out how to make all levels of care widely accessible to their citizens.
Brazil, for example, has a national public health system that emphasizes preventive, primary and urgent care services that are delivered at a community level. Brazilians have free community health care centers in each community; like our public school systems, patients can obtain a myriad of health services from routine screenings to medication refills and urgent appointments for sickness or mental health concerns.
Putting these foundational services directly into every community ensures people receive the level of care they need and can greatly reduce the need for costly emergency visits. It also signals a public commitment to prevention-focused primary care, which just about any health expert would agree is the most cost-efficient and effective way to keep a population healthy.
Adapting similar systems in the US is possible and plausible. We’ve actually already done it for emergency medicine services, where we’ve built a nationwide network of community-based centers that can be accessed just by dialing 911. We need to bring the same systems-level thinking to making preventive and primary care widely accessible and affordable.
Critics will say that we can’t afford such large-scale change in our health care system. But can we afford the current system?
When I see our emergency waiting rooms filling up with patients who are more desperate than sick, who wind up there because they have no other means to access health care, I wonder why we’re so willing to accept this status quo.
We are failing these patients, and it’s time for us to find the will to demand better.
Catherine A. Staton, MD, Msc, is an associate professor of Surgery and Global Health at Duke University and an emergency medicine physician with the Duke University Medical Center.
Join the tens of thousands of subscribers who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday newsletter, and please share the link with friends and colleagues: https://www.globalhealthnow.org/subscribe
Emergency room patients have to wait for treatment in the hallways of Atlanta’s Grady Memorial Hospital on July 29, 2006. Jonathan Torgovnik/Getty Images