State of the Science: Malaria Vaccines
More than 300 malaria vaccine experts from all over the world convened Tuesday—World Malaria Day—at a symposium in Baltimore sponsored by the Johns Hopkins Malaria Research Institute.
The gathering took place a day after blockbuster news broke on the malaria vaccine front. WHO announced on Monday that the world’s first malaria vaccine will be field-tested in pilot programs in Ghana, Kenya and Malawi in 2018.
WHO’s approval of pilots for the RTS,S vaccine (the first malaria vaccine to have successfully completed a Phase III clinical trial though it is only partially effective) is a milestone in the long and hard-fought search for a malaria vaccine.
Although the parasite annually kills an estimated 429,000 people and infects 212 million, global efforts against malaria have gained considerable momentum in recent years. Mortality rates have fallen by nearly 30% from 2010 to 2015 and incidence fell by 21% during the same period, according to WHO’s 2016 malaria report.
Infectious disease expert Ripley Ballou, who has had a leading role in the 30-year-plus development of the RTS,S vaccine, told the audience at the Johns Hopkins Bloomberg School of Public Health that the vaccine has the potential to have a “major public health impact.” When paired with other malaria control measures, it could save tens of thousands of lives in Africa, WHO announced.
The head of clinical research and translational science in the vaccines division at pharmaceutical company GSK, Ballou says that, based on predictive modeling, the vaccine—developed to protect children against the most deadly malaria parasite Plasmodium falciparum—can prevent 1 malaria death and 230 clinical malaria cases per 200 vaccinated children over a 15-year period.
The pilots will involve 750,000 children and will allow researchers to gain a fuller understanding of the vaccine’s benefits and risks in real-life settings. Ballou says that future goals are to expand the vaccine to protect against P. vivax and to increase its efficacy for use in mass vaccination campaigns.
Also sharing other promising research at the symposium was Stefan Kappe, from the Center for Infectious Disease Research in Seattle. Kappe focuses on the malaria parasite’s pre-erythrocytic stages, which occur after the mosquito bite but before the victim has symptoms of the disease. If a vaccine can be created to stop the parasite at this point, it both blocks infection and prevents transmission (by eliminating the parasite before it has a chance to reproduce in astonishing numbers and get picked up by a follow-up mosquito bite.)
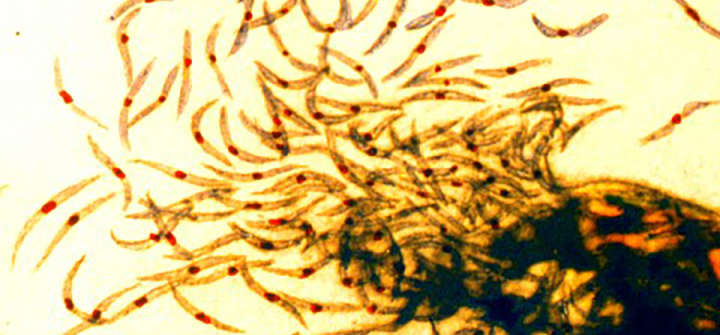
Kappe’s lab is investigating the use of genetically engineered P. falciparum sporozoites. (During the mosquito’s bite, a small number of sporozoites move from the mosquito’s salivary glands to its victim’s bloodstream and a few of those reach the liver where they hide out, transform themselves and multiply before bursting back into the bloodstream.) The PfGAP3KO vaccine has been shown to be safe in humans and protective in animal models, he said. An efficacy trial in humans is underway.
The advantage of the genetic engineering platform is that it can tweak vaccine strains to improve the vaccine, Kappe said. Additional work on the PfGAP vaccine may yield broader protection against other Plasmodium species, he said.
A vaccine that can protect people against the Plasmodium parasite—one of the great killers in human history—has frustrated scientists for decades, said conference organizer Fidel Zavala, a JHMRI faculty member, who began the day by explaining the history of the malaria vaccine quest. Zavala noted H.W. Mulligan’s research in the 1940s that used UV-attenuated sporozoites to successfully induce protection in birds. That was followed by studies of radiation-weakened parasites in mice and, in the 1970s, protection in humans using a vaccine based on Plasmodium sporozoites from irradiated mosquitoes, Zavala said.
Attendees were welcomed to the symposium by JHMRI director Peter Agre and Dean Michael J. Klag. “This is the largest group we’ve ever had for this symposium—around 350 registrants,” Klag said. “That growth mirrors the incredible investment and support for malaria over the last decade. With that tremendous support in field and lab research… we’ve seen advances like never before.”
The daylong symposium featured leading scientists, clinicians and public health and policy experts in the malaria field from top research institutions and schools in the US, Australia, Tanzania, the Netherlands, England and Colombia. Key symposium topics were Pre-erythrocytic Vaccines, Vaccines in Endemic Areas, Blood-stage Vaccines and Basic Aspects of Vaccinology. Speakers included:
Robert Seder (National Institutes of Health)
Robert Sauerwein (Radboud University, Netherlands)
Carole Long (National Institutes of Health)
Michael Good (Griffith University, Australia)
Simon Draper (Edward Jenner Institute for Vaccine Research, England)
Prakash Srinivasan (Johns Hopkins Bloomberg School of Public Health)
Patrick Duffy (National Institutes of Health)
Said Jongo (Ifakara Health Institute, Tanzania)
Susan Pierce (National Institutes of Health)
Eleanor Riley (London School of Hygiene and Tropical Medicine)
Peter Crompton (National Institutes of Health)
John T. Hardy (University of Iowa)
Dyann Wirth (Harvard T.H. Chan School of Public Health)
Malaria sporozoites, the infectious form of the malaria parasite that is injected into people by mosquitoes. Image/NIAID