Bitter Harvest: Cassava and Konzo, the Crippling Disease: Part I
Part 1: Desire’s Antidote to Poison
DEMOCRATIC REPUBLIC OF CONGO—Beads of sweat shimmer on Desire Tshala-Katumbay’s skin. His broad-shouldered body crunches behind the driver’s seat. “The sun is on my side,” Tshala says, squinting in the morning light. “Should the sun be on my side?”
Tshala’s question lingers unanswered as the jeep tumbles over sandy hills. Grasslands sparkle green. Fields turn into forests of slim trees. A row of teenagers in sand-stained T-shirts walk along the roadside, rifles slung across their shoulders. Before a rickety wooden bridge, Tshala steps out of the vehicle to speak with men at the river’s edge. Angola is on the other side, he reports. We’ve gone south instead of north. The detour means we’ll be on this back-breaking road deep into the pitch black night. Tshala knew the sun should not have been on his side, but now we’ve learned a lesson. Become a little more self-reliant.
Therapy is what Tshala jokingly calls the tortuous trip to Kahemba, a two-day drive from the capital of the eastern Democratic Republic of Congo. There, more than 3,500 people have been crippled by cyanide in their food, a condition called konzo. Roads are treacherous because infrastructure barely exists in the country, thanks to 2 decades of conflict, following 30 years of severe corruption and 80 years of colonization by Belgians who killed and tortured millions of Congolese. Running water, electricity and adequate health care are rare outside of the capital city of Kinshasa—not to mention the tools Tshala needs to study konzo’s underpinnings. For that, Tshala, a Congolese-born physician and neurotoxicologist at Oregon Health & Science University, returns to his laboratory in Portland. He keeps one foot in Kahemba, however. He tells me, “You cannot fix people’s problems if you do not talk with them and see what they experience.”
Very few scientists travel through the Congo. Tshala contends with that fact when he applies for research grants. His first challenge is always to convince funders and scientists that konzo exists. Even though the WHO describes the disease on their website, Tshala says people aren’t interested.
Meanwhile, most people afflicted by konzo aren’t aware of the science. Living in remote regions hardly touched by Western medicine, many people crippled by the disease never get to a hospital. That means their cases are not recorded. For this reason, konzo researchers consider the number of cases officially reported thus far in Africa—around 11,000—a massive underestimate (PLoS Neglected Tropical Diseases, 2011). On this trip, Tshala’s main goal is to bridge the gap between his worlds so that each side comes to understand the other. He’ll meet with the community in Kahemba, and then hold a scientific workshop in the capital. “If I had the means I could do a lot,” he says, “but even without the means, I can do something.”

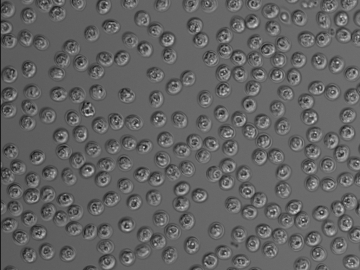
Belgian officials in Congo described konzo in the 1930s, but its cause went unknown for the next 50 years. That’s when Hans Rosling—now a world famous epidemiologist and statistician—witnessed an outbreak of the disease while he served as a doctor in Mozambique. Nuns at a nearby mission summoned him during a drought in 1983. They wrote that a growing number of people could no longer walk. After ruling out viruses and chemical weapons, Rosling linked the malady to populations who had nothing to eat except for bitter varieties of the staple crop, cassava. Urine samples from these patients contained a cyanide substance (thiocyanate), and flour made from cassava roots during the drought had 3 times as much cyanide (technically, cyanogenic glucoside) as usual. Subsequent studies have found that cassava roots grown in dry soil in the lab have 4 times more cyanide than well-watered plants of the same variety (Functional Plant Biology, 2013). Researchers suggest the plants produce the toxin to ward off pests who feed off their drought-weakened flesh.
Not wanting to damn a crop that millions of people safely eat, Rosling turned to a Congolese tribal name for the disease, konzo, also used to describe an antelope tethered at its knees. And he also identified poverty as a root cause of the condition because the people who had the disease, no matter where in Africa they were from, were susceptible to cassava’s toxin because they were malnourished. “All konzo communities are identical in extreme poverty,” he says.
Like Rosling, Tshala’s life changed with the vision of towns populated by skeleton-thin people hobbling and crawling down dirt roads. He studied konzo during his neurology residency at the University of Kinshasa, and dug deeper into the regions of the brain konzo alters during graduate school at the University of Uppsala in Sweden. Later, he worked on the molecules involved in cassava’s toxicity. Then he and his colleagues reported that cyanide in cassava may also cause cognitive problems—even when children don’t show outward signs of the disease.

Cassava roots dry on the roof of a house on the outskirts of Kahemba. Image by Neil Brandvold
“I’ve done the same cognitive tests with kids that had been near the coma state with cerebral malaria, and the long-term effects from that are nothing near on the level of what we see with konzo children,” says Michael Boivin, a neuropsychologist at Michigan State University who collaborates with Tshala. In 2013, researchers pinpointed one chemical underlying the cognitive damage (Pediatrics, 2013).
Late in the afternoon, we pull over into a village where white cassava roots line the hay roofs of houses. Women have soaked these roots in water and placed them in the sun to dry. A couple of adolescent girls beat the roots into flour with tall wooden rods. A crowd of people from the village congregate around our crew. Speaking in Lingala, a language common in this part of Congo, Tshala introduces himself and asks if they’ve heard of konzo. Blank stares. Then he imitates how a person with the disease hobbles and giggles break out. People from villages further down the road walk like that, they say.
Like people everywhere, the Congolese prefer conversations to instructions. Health officials in the country recognized this 20 years ago during a measles outbreak, when the population feared vaccination. “People refused because they thought measles was due to spirits and injections wouldn't help,” says Kasenya Sanika Ruffin, a 59-year-old who has no formal training but transmits messages between doctors and his neighborhood. In Congo, this person is called a “Relais Communautaire.”
“Measles became worse and it was death, death, death, death,” Ruffin recalls. “Hospitals were overflowing. So that’s when the health authorities said we need the Relais to talk with the community.” It worked. The outbreak fizzled out.
Ruffin walks with a severe limp due to konzo. Like most people in the area, he blamed his condition on sorcery until, around 1998, a doctor showed him photos of others with the disease around the continent and said that they too had consumed bitter cassava. “That’s when I realized that konzo was a disease and not witchcraft,” he says. “It was such a relief because if it’s not a curse, something can be done to prevent it.”
Obvious as it seems, earnest dialogue can be hard to come by. Veteran Ebola hunter, Jean-Jacques Muembe-Tamfum, investigated the Ebola outbreaks in Congo in 1976 and 1995. “I engaged the community immediately,” Tamfum tells me in his office in Kinshasa, where he directs the National Institute of Biomedical Research. He thinks this is the primary mistake made during the most recent crisis in West Africa. “I went to Liberia during the Ebola outbreak,” he says, “and health officials were not having conversations with people.”

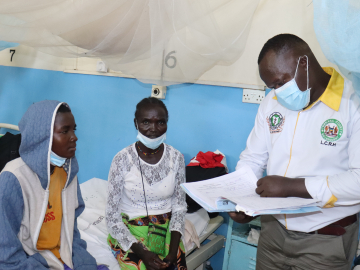
Desire Tshala addressing Kahemba officials about konzo. Image by Amy Maxmen
Night has fallen when we arrive in Kahemba. A couple of women put pots of stew and cassava—prepared as a starchy white lump called fufu—on the table for dinner in the house where Tshala stays while in town. In the pale orange haze of the morning, women walk through fields with baskets on their heads. Children kick a deflated soccer ball. And it seems that roughly 1 in 10 people I see holds themselves up on makeshift crutches or sits on the ground and on benches with crooked legs beneath them.
Dressed in a navy T-shirt with a United States of America logo, Tshala heads to Kahemba’s health center, a sparsely furnished, concrete building. He speaks with a nutritionist, Diendonne Kasenya, who emphasizes the need to raise awareness of konzo in Kahemba. “Poverty causes konzo,” Kasenya tells me. “And konzo generates poverty because the affected person cannot farm, and they are absolutely dependent on their family, who will spend any money they have to care for them.”
At noon, a dozen health workers, three WHO officials and some of Kahemba’s leaders gather at the center to hear Tshala speak. He begins: “Since I have worked here for six or seven years, I feel it is my moral responsibility to tell you what I have learned.” He explains how Kahemba is not unique, even though some refer to the town as the capital of konzo, as a city of suffering. He explains how scientists have looked for alternative explanations for paralysis. They tested soil, water, urine and blood for signs of metals, battery acid or pathogenic viruses and bacteria. Nothing was abnormal. Tshala turns toward a blackboard and writes, “50-200ppm.” It’s the amount of cyanide detected in cassava flour from Kahemba. According to the WHO, he says, people should not consume products with more than 10ppm. Next he says urine samples from people in Kahemba contained 8 to 10 times more thiocyanate (a marker of cyanide) than what’s considered normal.
The good news, Tshala adds, is that cassava’s toxicity is reduced when its roots are soaked in water for several days before they are eaten. And he says beans, fish and other proteins help the body detoxify the plant. He repeats this message to people all day. At times, the conversations grow tense. People say they have no other food, so how can he expect them to eat a varied diet. They say they haven’t eaten all day, so how can he expect them to soak their cassava roots for a week. “It’s very difficult because I have nothing to offer,” Tshala tells me later. “I cannot be a benefactor to the town.”
Other solutions require outside intervention from scientists, the government or aid workers who could donate farm tools, fertilizer, irrigation and livestock. But none of these are forthcoming—and if they were, they’re often unsustainable. “As a Congolese,” he says, “I’m telling you that the solutions must come from you.”
A day before I leave from Kinshasa, Tshala meets me for coffee. We talk about the factors dragging Kahemba down, such as its distance from markets, its increasingly poor soil, and the worn-down and defeated mindsets of those who live there. “The solution to konzo seems simple, but it is not simple,” Tshala says. “Konzo is the tip of the iceberg, but so much is going on below the water.”
Read the Intro to the Series.
Special thanks to the Pulitzer Center on Crisis Reporting for supporting photography for this series.
Join the thousands of subscribers who rely on Global Health NOW summaries and exclusive articles for the latest public health news. Sign up for our free weekday enewsletter, and please share the link with friends and colleagues: Subscribe to GHN